Prevalence And Factors Associated with Postpartum Female Sexual Dysfunction in Muyinga Province, Burundi
Nininahazwe L1, Adesina O2, Appiah S C Y3
1. Department of Obstetrics and Gynaecology, Pan African University Life and Earth Sciences Institute (Including Health and Agriculture) PAULESI
University College Hospital / University of Ibadan, Ibadan Nigeria.
2. Dept of Obstetrics and Gynaecology, University of Ibadan, National Maternal and Child Health, University of Ibadan; Reproductive Health Program, PAULESI.
3. Department of Sociology and Social Work, Kwame Nkrumah University of Science and Technology; 233249478809; scyappiah@knust.edu.gh
Corresponding Author:
Landes Nininahazwe
Muyinga, Burundi
Phone numbers: (+257)62864820E- nilandes95@gmail.com
ABSTRACT
Background: Female sexual dysfunction is a major problem that affects 30-78% of women. Objectives: The purpose of this study was to determine the prevalence and factors associated with postpartum sexual dysfunction among women in Muyinga province, Burundi. Methods: The study was cross-sectional among women aged between 18 – 49 years, who are in 3-12 months postpartum. A multistage random sampling technic was used to select 415 women attending primary health centres with a questionnaire including sociodemographic characteristics, obstetric conditions, postpartum period, and sexual function. Sexual function was assessed using Female Sexual Function Index. Data was entered into Statistical Package for Social Scientists version 22 for analysis with statistical significance set at 5%. Chi-square test for analyzing factors associated with sexual dysfunction. Logistic regression was used to analyze predictive factors of sexual dysfunction. Female dysfunction was identified with an FSFI score ≤26.55. Results: The mean age was 27 (SD±6.53) years. 274 (66%) reported sexual dysfunction with a total score of Female Sexual Function index of 25.11±3.90. Sexual dysfunction was identified as the sexual desire at 90.6%, sexual arousal at 62.9%, lubrication at 29.2%, and orgasm at 49.9%. Factors associated with sexual dysfunction (p<0.05) were the type of contraceptive methods, residence, and delivery place. Predictive factors were the age of the respondent (aOR: 0.3 (95% CI: 0.10-0.89); P = 0.030), residence (aOR: 3.4 (95% CI: 2.13-5.54); P= 0.000), sexual resumption time (aOR: 1.8 (95% CI: 1.12-2.99); P=0.015), postpartum period (aOR: 0.59 (95% CI: 0.37-0.94); P=0.029), DMPA use (aOR: 0.45 (95% CI: 0.27- 0.75); P=0.002). Conclusion: FSD is very noticeable in the postpartum period. Hence an open discussion is beneficial between partners and healthcare professionals should also offer guidance in addition to suggesting various therapy alternatives.
Keywords: postpartum, sexual dysfunction, female sexual function index, Muyinga, Burundi
INTRODUCTION
The evaluation of sexual intercourse resumption has been recommended by the World Health Organization (WHO) for women in their early postpartum period.1 The occurrences of body changes after childbirth have an impact on women's health, as well as other parts of their lives, such as sexual activity, which is important in human life.2 The causes of Female Sexual Dysfunction are multifaceted involving, among others, mental health conditions, surgery, obstetrical and gynaecological illnesses, and chronic diseases including diabetes. Pregnancy, childbirth, and postpartum variables are among the most crucial of these.3 The study reported that sexual organs are affected differently by the mode of delivery, and genital abnormalities might lead to sexual dysfunctions, women experience issues including painful sex, a decline in desire, a dry vagina, and an inability to experience orgasm after giving birth.4 In addition to discomfort, female sexual desire, arousal, and orgasmic disorders are complicated topics since they include elements of a subjective intercourse experience.5 A study revealed the existence of vaginismus before pregnancy, dyspareunia during pregnancy, vaginal delivery with episiotomy and religious affiliation were found to be associated factors with postpartum sexual dysfunction.6 Menarche and menopause are the beginning and end of womanhood because they are characteristics of the ability to reproduce and have a close evolutionary connection to sexual function.7 The early resumption of sexual activity after childbirth has a significantly higher risk of developing infections and sexual dysfunction because of vaginal lesions and abrasions.8 Additionally, the use of contraceptive methods particularly hormonal contraception, have the potential to have an impact on how women respond sexually and the possible dangers and benefits of contraception for a female sexual function should be considered when considering a woman's decision to engage in sexual activity outside of pregnancy.9 This study was conducted to determine the prevalence and factors associated with postpartum sexual dysfunction among women in Muyinga province, Burundi.
MATERIAL AND METHODS
It was a descriptive cross-section study conducted in Muyinga province, Burundi between April to June 2022 in primary health centres of the district sanitary of Muyinga and Gashoho. Participants in 3-12 months of postpartum attending primary health centres and who consent to be interviewed were recruited. A multistage random technique was used to select respondents. Urban and rural in the first stage, 6 primary health centres in two district sanitary were considered. The sample was consecutive including postpartum women who fulfilled the following inclusion criteria: women resident in Muyinga province, aged between 18 – 49 years, and who had given birth during the previous 3-12 months. The sample was calculated using the following formula and assuming a 10% non-responsiveness rate, 415 women were recruited.
n= [Z²*p(1-p)]/d²
The questionnaire reviewed and validated was used to assess four sections: sociodemographic characteristics, obstetrics, postpartum conditions, and female sexual function. Index of Female Sexual Function is a survey of 19 questions that evaluate six domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain. Each domain was assessed by related questions; sexual desire (frequency and level), arousal (frequency, level, confidence and satisfaction), lubrication (frequency, difficulty, frequency to maintain lubrication and difficulty to maintain lubrication), orgasm (frequency, difficulty of reaching orgasm and satisfaction), satisfaction (closeness of spouse, overall sexual life and sexual relationship) and pain (pain frequency during vaginal penetration, pain frequency following vaginal penetration and pain level during penetration).10
Collected data were analysed using Statistical Package for Social Scientists version 22 with a p-value set at 5%. Pearson Chi-square test and logistic regression analysis were performed to analyse associated and predict factors respectively. For the female sexual function index, the scale was rated from 1 to 5 for questions 1,2, the remaining rate was from 0 to 5. The score of each participant was calculated by summing responses that compose each domain and multiplying by the domain factor which was 0.6 for sexual desire, 0.3 for arousal and lubrication, and 0.4 for orgasm, satisfaction, and pain. A participant who had a total score ≤ 26.55 was considered as having a sexual dysfunction.
The study's ethical approval came from the University College Hospital/University of Ibadan Ethics Committee. Before beginning data collection, permission to perform the study was requested from the Minister of Public Health, the Health Office of the Province, and the District Sanitary Office in Burundi.
RESULTS
Four hundred and fifteen women were recruited in this study. Sexual dysfunction was detected in 274 (66%) of the studied women (Table 3).
Table 1: Socio-demographic characteristics of participants
|
Variable |
Frequency |
(%) |
|
Age group |
Mean ±SD = 27±6.53 |
|
|
<=20 |
54 |
13.0 |
|
21-25 |
126 |
30.4 |
|
26-30 |
105 |
25.3 |
|
31-35 |
76 |
18.3 |
|
36-40 |
36 |
8.7 |
|
41-45 |
15 |
3.6 |
|
46-49 |
3 |
0.7 |
|
Residence |
|
|
|
Urban |
182 |
43.9 |
|
Rural |
233 |
56.1 |
|
Marital status |
|
|
|
Single |
9 |
2.2 |
|
Married |
400 |
96.4 |
|
Consensual Union |
1 |
0.2 |
|
Separated |
5 |
1.2 |
|
Education level of the respondent |
|
|
|
No formal education |
139 |
33.5 |
|
Primary |
172 |
41.4 |
|
Lower Secondary and above |
104 |
25.1 |
|
Occupation of the respondent |
|
|
|
Unemployed |
16 |
3.8 |
|
Employed public sector |
21 |
5.1 |
|
Farmer |
269 |
64.8 |
|
Other work |
109 |
26.3 |
Table 2: Obstetric and postpartum conditions of participants
|
Variable |
Frequency |
% |
|
Chronic medical illness |
|
|
|
Yes |
17 |
4.1 |
|
No |
398 |
95.9 |
|
BMI |
||
|
Underweight (BMI<18.5) |
25 |
6 |
|
Normal (BMI: 18.5-24.9) |
385 |
92.8 |
|
Overweight (BMI: 25-29.9) |
5 |
1.2 |
|
Gestational age at delivery |
39.13±1.622 |
|
|
Before term (<37 weeks) |
6 |
1.4 |
|
Term (37-42 weeks) |
395 |
95.2 |
|
Over term (>42 weeks) |
14 |
3.4 |
|
Delivery place |
|
|
|
Primary Health Centre |
160 |
38.6 |
|
District hospital |
246 |
59.3 |
|
Regional hospital |
4 |
1 |
|
Home |
5 |
1.2 |
|
Mode of delivery |
|
|
|
Vaginal delivery |
364 |
87.7 |
|
Caesarean |
51 |
12.3 |
|
Complications during pregnancy |
|
|
|
Yes |
61 |
14.7 |
|
Complications during labour |
|
|
|
Yes |
19 |
4.6 |
|
Complications after delivery |
|
|
|
Yes |
39 |
9.4 |
|
Post-partum period (months) |
7.98±2.99 |
|
|
3-6 |
149 |
35.9 |
|
>6-9 |
127 |
30.6 |
|
>9-12 |
139 |
33.5 |
|
Use of FP method |
|
|
|
Yes |
289 |
69.6 |
|
No |
126 |
30.4 |
|
Type of FP method |
|
|
|
IUD |
8 |
2.8 |
|
DMPA |
142 |
49.1 |
|
COC |
4 |
1.4 |
|
COP |
11 |
3.8 |
|
Emergency Contraceptive Pills |
1 |
0.3 |
|
Implant |
38 |
13.1 |
|
Condom |
10 |
3.5 |
|
Beads |
21 |
7.3 |
|
Natural method |
54 |
18.7 |
|
Category of FP method |
|
|
|
Hormonal Contraceptives |
196 |
67.8 |
|
Non-hormonal Contraceptives |
93 |
32.2 |
|
Sexual intercourse resumption |
5.11±3.879 |
|
|
1 week or less |
41 |
9.9 |
|
Within 1-6 weeks |
258 |
62.2 |
|
After 6 weeks |
116 |
28 |
Table 3: Prevalence of postpartum sexual dysfunction among participants
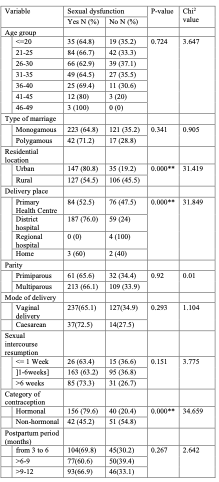
Table 4: Factors associated with sexual dysfunction among participants.
The mean age was 27 (SD±6.53) years with the age groups of 21-25 and 26-30 years having the highest proportions of respondents accounting for 30.4% and 25.3%, respectively. Over half (56.1%) of respondents were urban residents. Nearly all (96.4%) of them were married while 85.4% of them were in a monogamous marriage, 41.4% of women had attended the primary level of education while 33.5% never attended any formal education, and 64.8% were involved in farming as the main occupation (Table 1).
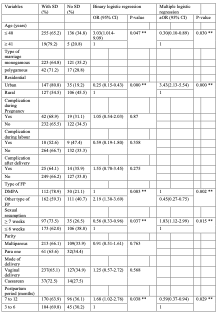
Table 5: Logistic regression predictors of sexual dysfunction
Only 17 respondents reportedly had a chronic medical illness, 92.8% had a normal body mass index, the majority (95.2%) of respondents gave birth when the pregnancy was within the normal term (37-42 weeks), 59.3% gave birth in district hospitals, 77.6% were multiparous, vaginal delivery was the mode of delivery in 87.7% (Table 2).
The postpartum period of women surveyed was comprised of between 3 and 12 months with nearly 36% of women within 3-6 months. 69.6% use contraceptive methods. Hormonal contraceptives were used by 67.2%, the most common contraceptive method was found to be DMPA (49.1%). The majority of women (62.2%) resumed sexual intercourse between the first and sixth week, and nearly one in ten women had sex within the first week after delivery (Table 2).
Based on the total cut-off score of FSFI in the studied population, 66% reported female sexual dysfunction. The most prevalent dysfunction among women was the frequency of sexual desire (90.6%) followed by sexual arousal (62.9%) and orgasm (49.9%). Lubrification, satisfaction and pain were the least prevalent dysfunctions with 29.4%, 29.2% and 17.8% respectively (Table 3).
Factors significantly associated with FSD were found to be the residential location (p=0.000, X2 = 31.4), delivery place (p=0.000, X2 = 31.8) and type of the contraceptive method (p=0.000, X2 = 19.3) (Table 4). The variables which predicted sexual dysfunction in the binary logistic regression model were included in the multiple logistic regression to show the effects of individual predictors while adjusting for other predictor variables. The input variables to the model included age, residence, type of contraceptive methods, postpartum period, and sexual intercourse resumption. FSD was found to be predicted in women who are aged more than 41 years (aOR:0.30(95%; CI:0.10-0.89 p=0.030), live in the urban area (aOR: 3.43(95%; CI: (2.13-5.54) p=0.000), used DMPA contraception (aOR : 0.45(95%; CI(0.27-0.75) p=0.002), resumed sexual intercourse within 6 weeks after childbirth (aOR: 1.83(95%; CI(1.12-2.99) p=0.015), were in the 3 - 6 months of postpartum ( aOR: 0.59 (95%; CI:(0.37-0.94) p=0.029) (Table 5).
DISCUSSION
The prevalence of sexual dysfunction among women in the postpartum period was funded to be 66%. This result is in line with the study conducted in Turkey among women who are in their 12 months of postpartum which reported that 67.6% of participants had postpartum sexual dysfunction.11 This prevalence is lower than the one reported in Egypt 74.7%,12 Turkey 74.3%,13 but it is much higher compared to the study conducted in South West Ethiopia 53.3%,14 Brasilia 58.3%,15 Iran 46.2%.16 Results of the prevalence of sexual dysfunction from various studies are different and this may also result from the varying mode of assessing sexual function among participants and the sample size.
In the present study, 90.6% have sexual desire problems and 62.9% had arousal problems. Our findings are contrary to the one done among postpartum women on the East Coast of Malaysia which shows that the most problem is lubrication (85.6%) and desire 69.7%.17 In Iran, it has been revelated that sexual desire was the most sexual function problem (45.3%) and satisfaction problem in 44.5% of 400 women surveyed.16 Maaita et al revealed that the most sexual impairment in the sexual function experienced by women was sexual desire with 49.4%, pain was not found prevalent in the population studied.18However, a study conducted among 398 participants using the Changes in Sexual Functioning Questionnaire-fourteen items (CSFQ-14) as a tool to assess sexual function, revealed that the prevalence of sexual dysfunction was 53.3%, sexual desire was dominant among the sexual dysfunction domain with 46.5%.14 On the other hand, orgasm and desire were reported as the most sexual dysfunction in 49.2%, and 45.5% respectively in a study population of 509 women.19 A previous study conducted in Australia has shown that sexual desire disorder (81.2%), orgasmic issues (53.5%), and sexual arousal disorder (52.3%) were the common sexual problem reported by postpartum women.20
Variables found to be significant predictors of sexual dysfunction among women in the postpartum period were age, postpartum period, residential location, time of sexual intercourse resumption, and type of contraceptive methods used. These findings are in the same line as those found in Upper Egypt where among the predictor factors of female sexual dysfunction there were age and use of contraceptive methods.21 Women aged more than 40 years were more likely to have sexual dysfunction than those aged less than 40 (aOR:0.30; 95% CI: 0.10-0.89 P=0.030). Similarly, Asefa et al., and Ibrahim et al. reported the same results.14, 19. The growth of a human body is characterized by many changes which are physical, psychological, and physiological, hormonal changes may lead to a decrease in sexual interest thus sexual dysfunction. Cross-sectional studies also confirmed the age of participants as a significant predictor of sexual dysfunction.16], 22,23. In contrast, another study reported no significant association between age and sexual dysfunction and age is not a factor that predicted sexual dysfunction.13, 15, 17. Literally, it is stated that female sexual function problem has a variety of causes, particularly during the first six months following childbirth. One of the causes is the hypo-oestrogenic condition which is based on a high level of prolactin in a breastfeeding woman and leads to vaginal dryness thus decreased of sexual desire and sexual function.17This goes in the same line as the result of the present study where women who were in their six months after delivery were more likely to have sexual dysfunction than those in more than six months (aOR:0.59; 95% CI: 0.37-0.94). In addition, according to the Institute of Statistics and Economic Studies of Burundi, in Muyinga province exclusive breastfeeding in the first six months is 93,8%.24 Saleh et al found that women in the first six months of postpartum had a higher risk of sexual dysfunction than those beyond six months.25 In another cross-sectional descriptive study, it was reported that among women with vaginal delivery and caesarean section, both during their first six months of the postpartum period, they had sexual function problems in all domains except desire.11
According to the result of this study, women who resume sexual intercourse before 6 weeks were more likely to have sexual dysfunction than those resuming after 6 weeks. A study conducted in Uganda showed that in some cases early sexual intercourse resumption was the factor of dyspareunia and this might be explained by social and cultural factors where resuming sexual intercourse early prevent partners from engaging in extramarital relationships.26 Resuming sexual activity before the scheduled period might hurt a woman’s health as her body changes are still ongoing.4 Even though many women around the world may not have sexual desire, they resume sexual activity within six weeks after giving birth to preserve the intimate relationship and for additional purposes, for instance, to satisfy their partners' desires or to prevent possible interpersonal conflicts that could result from a difference in sexual needs.27]
Notably, this study reported that the use of hormonal contraceptive methods especially DMPA was significantly predicting sexual function problems (p=0.002). A previous cross-sectional study conducted in Kenya reported that the use of hormonal contraceptive methods had a significant effect on female sexual dysfunction adjusted odds ratio: 2.695 (1.869–3.886, p < 0.0001).[28] In the same point of view, an Egyptian study mentioned that women who were using DMPA were more likely to have a problem with female sexual function.29 Consistent with previous studies that reported women who use hormonal contraceptives were more likely to experience a high level of lubrication problems, pain during sexual intercourse, and low level of sexual interest and orgasm than those who used non-hormonal.30–32. In this study, women living in urban areas were more likely to experience sexual function problems than those living in rural areas. According to the DHS 2017, injectable contraception use is most prevalent (12%) in urban areas than in rural areas for married and unmarried women this could explain why women in urban areas were more likely to have sexual dysfunction.33 On contrary, it has been reported that there was no prediction between residence and sexual dysfunction.34
According to the results of the present study, the mode of delivery in both women who had a vaginal delivery or caesarean section was not significantly predicting sexual dysfunction. This result is in line with the one reported from a cross-sectional study where women with normal childbirth and those with caesarean sections did not report postpartum sexual dysfunction.25When comparing these findings to the recent literature, our results are discordant with other studies that reported women who gave birth normally with episiotomy were more likely to experience sexual function impairment than those with caesarean section.6 Lurie et al. revealed that in each domain of the sexual function index, the score of each domain decreased as the postpartum period increased and there were no disparities in the mode of delivery.35 This suggests more research to be conducted.
CONCLUSION
The results of this study under consideration appear to suggest that family planning, employment status, delivery place, type of marriage, body mass index and residence may have an impact on various domains of female sexual function. In the logistic regression, the age of the participant, postpartum period, residential location, time of sexual intercourse resumption after childbirth, and type of contraceptive methods used was identified as statistically significant factors that predict sexual dysfunction among women in the postpartum period. This underlines the need of acknowledging as a serious public health issue and necessitates additional intervention and study.
Strengths and limitation of the study
Financial support and sponsorship
Africa Union Council
Pan African University
Conflict of interest
There is no conflict of interest
REFERENCES
 S. Martella, M. Rossi, L. Tiranini, and E. Martini, “Female sexual dysfunction (FSD): prevalence and impact on quality of life (QoL),” Maturitas, 2016, doi: 10.1016/j.maturitas.2016.09.013.
S. Martella, M. Rossi, L. Tiranini, and E. Martini, “Female sexual dysfunction (FSD): prevalence and impact on quality of life (QoL),” Maturitas, 2016, doi: 10.1016/j.maturitas.2016.09.013.