Dr. Adewole Ayodele Stephen
Department of Obstetrics &Gynaecology,
University of Medical Sciences, Ondo City, Ondo State.
ayospinene@yahoo.com,
aadewole@unimed.edu.ng
+234 803 650 1825
INTRODUCTION
It is commonplace that most women who have completed their family size and who present with symptomatic uterine fibroids will elect to have a hysterectomy operation done on them. In over 90% of the cases, the histological report comes as leiomyomata with or without hyaline degeneration.
It is rare for the histology report to come as Cavernous haemangioma.
Haemangiomas are simply described as benign tumors of blood vessels, and they commonly seen in the face, scalp, back or chest. They rarely arise in the uterus; however, they cause many symptoms such as abdominal pain and excessive vaginal bleeding. Haemangiomas can affect women of all ages and symptoms range from mild to severe, often times being misdiagnosed as other clinical conditions.
A cavernous haemangioma located in the uterus is a rare condition and very few incidents have been reported in the literature. A number of such uterine haemangiomas have been detected in pregnant women with complications such as uncontrolled vaginal bleeding or uterine pain.
In this case, we describe a cavernous haemangioma arising in a uterine intramural leiomyoma detected in a non-pregnant woman. To our knowledge, this case is unique in this environment because it has never been reported in South-Western Nigeria in any of the literatures located.
CASE REPORT
A 43-year-old Para 4+0 4 alive parturient woman was rushed to the Gynaecological Emergency Unit of the University of Medical Sciences Teaching Hospital, Ondo, on the 12th of December 2020 with a three years history of abdominal swelling, heavy vaginal bleeding and occasional abdominal pains. She was diagnosed as having co-existing uterine fibroids with her last pregnancy occurring two years prior to her hospitalization. She further stated that she experienced menorrhagia and dysmenorrhea since her last delivery. On physical examination of the patient, she was a young woman who was well hydrated and not ill-looking. She weighed 78 kg and with a height of 1.67 meters. Her Body Mass Index was 27.974 kg/m2. She was not febrile to touch, not pale, anicteric and she had no peripheral lymphadenopathy nor pedal edema. Her chest examination findings were normal. Her pulse rate was 84 beats per minute and they were regular, good volume pulses. Her blood pressure was 124/77mmHg. Her other cardiovascular findings were normal. Her respiratory rate was 17 cycles per minute. Her chest examination findings were normal. Her abdominal examination revealed suprapubic fullness. Her abdomen moved with respiration. There were no scarification marks and her umbilicus was flat. There were no areas of tenderness. There were no palpable hepato-splenomegaly. Her kidneys were not ballotable. There was an evidently palpable suprapubic mass even after patient has emptied her urinary bladder. The mass is commensurate with a 22-week uterine size. The suprapubic mass was mobile from side to side, and there was no evidence that the mass was attached to overlying tissues. There was no ascites on percussion and no bruit was heard over the mass on auscultation. Pelvic examination with speculum revealed a small cervical polyp projecting through the external cervical os into the vagina. The vaginal walls were grossly normal. Apart from the small cervical polyp, the overall outlook of the cervix was normal. The digital pelvic examination essentially demonstrated a bulky uterus. The cervical excitation was negative. The adnexa felt normal. The Pouch of Douglas felt normal.
The working diagnosis is uterine fibroids and fibroid polyp, with menorrhagia. Some of the investigations done included a Pelvic Ultrasonography which revealed a 5.5×5.0 cm mass with cystic components originating from the endometrium of the uterus and compressing the endometrial cavity. Her packed cell volume was 28% and as such there was no need for blood transfusion. She was counselled for total abdominal hysterectomy and bilateral salpingo-oophorectomy. The patient elected to have a total abdominal hysterectomy and bilateral salpingo-oophorectomy, and she therefore had full pre-operative work up for the surgery. The surgery was scheduled to take place on Monday, 21st of December 2020. This was nine days after she first presented at the Gynaecological Emergency Unit. The patient was admitted on Sunday, 20th December 2020 and had a pre-operative ward round done on her as well as other patients scheduled for surgery the next day, and the teams from the Anesthesiology Unit as well as the Obstetrics and Gynaecology Unit conducted the pre-operative Ward Round.
The patient underwent total abdominal hysterectomy due to excessive vaginal bleeding and the working diagnosis of multiple uterine fibroids and fibroid polyp. The surgery was done following the standard total abdominal hysterectomy procedure.
She had an essentially uneventful post-operative period and was placed on intravenous normal saline infusions alternated with 5% Dextrose Saline infusions, Co-Amoxiclav injections, metronidazole injections, Pentazocine Injections (with promethazine injections to potentiate the effect of the former), Paracetamol Injections, Diclofenac Injections, and other supportive parenteral medications. She recovered fully and all medications were changed to oral medications: Augmentin tablets, Metronidazole Tablets, Astymin Capsules, and Paracetamol tablets; she was subsequently discharged home after three days on admission, on the 24th of December 2020.
The hysterectomy and bilateral salpingo-oophorectomy samples were sent to the histopathology Department of the UNIMED Teaching Hospital and the results were as seen and documented by the consultant pathologist with the Anatomic Pathology Department of University of Medical Sciences Teaching Hospital, below:
Histopathology Report
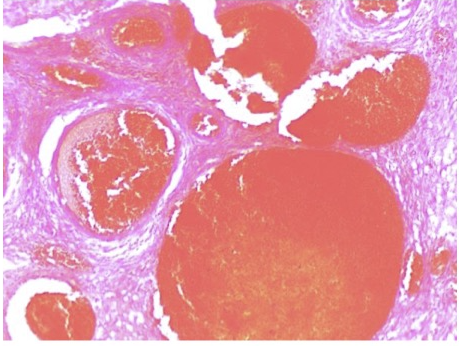
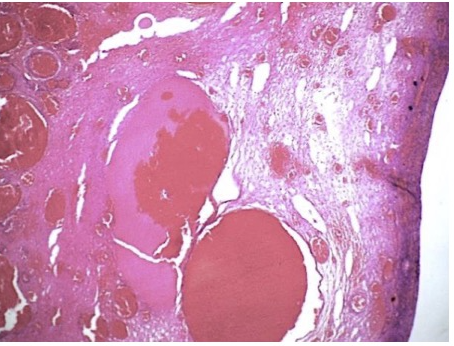
Upon gross examination of the hysterectomy sample, the uterus was seen, also a 2.0×1.5 cm polyp in the endocervical region and a 5.5×5.0 cm gray-tan colored intramural nodule with smooth borders in the uterine corpus were seen. There was a 1.4×1.1 cm area containing blood-filled cystic spaces on the cut surface of the nodule.

Gross hysterectomy specimen showing engorged vascular spaces at the lower uterine segment
Cut sections show a patent endometrial cavity. There is a polypoid necrotic greyish white mass which is foul-smelling and appears to arise from the lower segment of the uterus. The cervix is recognizable and appears grossly normal. Cut sections through this polypoid mass show a grayish white appearance with multiple foci of haemorrhage and necrosis. The outer anterior surface of the lower segment of the uterus appears to be perforated by an intra-parenchymal extension of this polypoid mass. The left fallopian tube measures 7cm in length and 1cm in its widest diameter. There is a para-tubal cyst
located at the isthmus of the fallopian tube. Cut sections through the fallopian tube shows a patent cavity. The left ovary is firm in consistency and measures 4 x 2.5 x 1.5cm. Cut sections show a greyish white appearance with follicles seen. The right fallopian tube measures 9cm in length and 1cm in its widest diameter. Cut sections show a patent lumen. The right ovary is firm in consistency and measures 4 x 4 x 2cm. Cut sections show a haemorrhagic appearance.
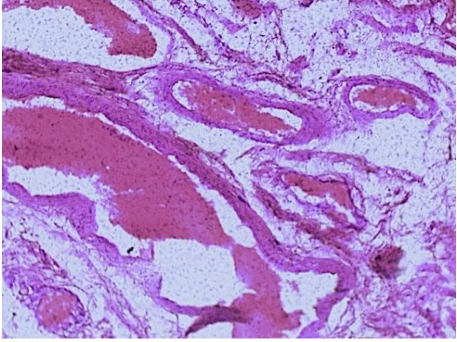
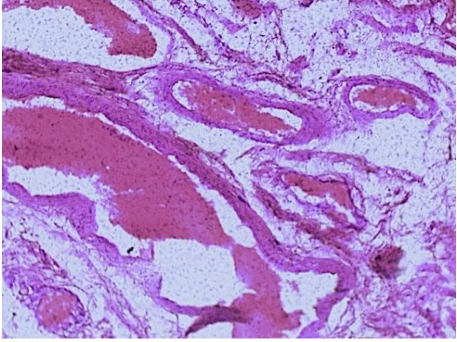
H and E stains with cavernouusly dilated blood vessels
The histologic sections show a proliferative phase endometrium. The lower uterine segment Sections show a benign lesion composed of dilated anastomosing cavernous channels, a few are congested within the fibro-collagenous stroma of the uterus interspersed with the smooth muscle fascicles. Also seen are adjacent vascular capillary beds which appear to connect with these channels. There was no focus of atypia, atypical mitosis, necrosis or endothelial multi-layering is seen.
The overall features are in keeping with a Cavernous Uterine Haemangioma. Histologic sections of the right and left Fallopian tubes show plicae disposed in papillae supported by fibro-collagenous stroma and lined by ciliated columnar cells. The left fallopian tube shows a cystic lesion lined by ciliated columnar cells and containing eosinophilic secretions. No focus of atypia or malignancy is seen. Features are in keeping with normal fallopian tube tissue with a left para-tubal cyst. Sections of the right ovary show ovarian tissue with atretic follicles within a well vascularized fibroblastic stroma. A functional cyst is seen. Also seen is a hemorrhagic cystic lesion lined by an outer
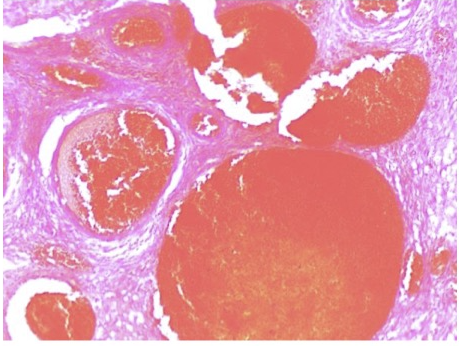
H and E stain section showing cavernously dilated vessels
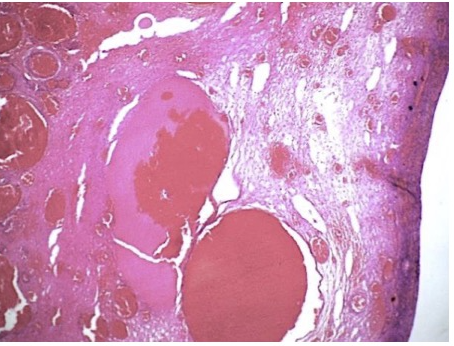
H and E stain section showing relationship between cavernously dilated vessels and lower uterine segment
layer of luteinized theca cells and an inner layer of granulation tissue. Overall features are in keeping with a Hemorrhagic Corpus Luteum Cyst. Histologic sections of the left ovary show ovarian tissue with atretic follicles within a well vascularized fibroblastic stroma. A functional cyst is seen. Overall features are in keeping with normal ovarian tissue.
DISCUSSION
Diverse varieties of clinically significant vascular lesions have been described in the uterus, which include capillary and cavernous haemangiomas, arterio-venous malformations, angiomyomas, and hemangioendotheliomas. 1 They can be congenital or acquired. There have been rare case reports of uterine haemangiomas associated with hereditary syndromes such as Hereditary Hemorrhagic Telangiectasia and Klippel–Trénaunay–Weber syndrome. 2 In this case the woman presented with what was diagnosed as uterine fibroids all the while until she had her surgery for menorrhagia secondary to uterine fibroids. There is no literature to show that this type of case has been previously reported in South Western Nigeria.
Majority of the cases reported in literature were found in women who were either pregnant or were in their immediate postpartum period. This index case was an exception as she hitherto had uneventful antenatal and postpartum period in all her deliveries. She only had an ultrasound diagnosis of uterine fibroids in her last pregnancy, and only began having menorrhagia after her last confinement, which has spanned two years prior to her presentation at the Gynaecological Emergency Unit. One case of large arterio-venous malformation of the uterus was described in a pregnant woman with Mullerian system hypoplasia.3The haemangiomas of the uterus can be found in any age group without predominance in any decade. The youngest patient described in literature was a 14-year-old girl who had to go undergo hysterectomy for the life-threatening bleeding. 4
The haemangiomas can involve either the uterine corpus or the cervix. In this index case it involved the uterine corpus which appears to be the more favoured site. They can be diffuse or localized. The localized haemangioma can present as endometrial polyp (as in the index case) or it can be localized with in the myometrium. Diffuse haemangiomas commonly involve the entire thickness of the uterine wall extending from the endometrium to the serosa. In literature, very few cases of diffuse cavernous haemangioma have been described in pregnant women till date. 5 They all commonly present with uncontrollable antepartum or post-partum haemorrhage and a few might have died as a result of the haemorrhage. 6
Cavernous Haemangiomas carry a significant risk for the mother as well as for the baby, as described in the initial case reports where only one out of four neonates could be saved. There has been single case report of uterine rupture also. 7 The diagnosis of the haemangioma is not usually suspected clinically due to the rarity of the condition and absence of any specific clinical features. However, antenatal diagnosis could be established with ultrasonography in four cases. 8
The characteristic imaging findings described in the literature are tubular echolucent spaces present throughout the myometrium without any blood flow by color Doppler. Magnetic resonance imaging (MRI) has also been used as an additional imaging modality to diagnose it. 9 The other imaging techniques that can be helpful in the diagnosis are arteriography and computed topography (CT) scan, although their usefulness is limited during the pregnancy. The histopathological examination is the gold standard to confirm the diagnosis.
Histologically, uterine haemangiomas can be categorized as capillary type or cavernous type. The capillary haemangiomas demonstrate small size capillary vessels and are usually localized to the endometrium. The cavernous haemangiomas are composed of large dilated vascular channels and diffusely involve the uterus. Rarely, they can present as cavernous haemangiomatous polyp. 10 These lesions can be complicated by the thrombosis and sometimes calcification. Although, characteristic radiological findings have been described in the literature, much has not been described in terms of histology.
Hysterectomy has been the most common treatment for the diffuse uterine haemangiomas in the past for the uncontrollable bleeding. Even prophylactic hysterectomy has been done in the past to prevent the rupture during pregnancy. But it has been shown that with conservative management and vigilant approach, successful pregnancy can be done without resorting to the hysterectomy. 11 In addition, uterine artery embolization or internal artery ligation could be the alternative therapeutic approaches. These modalities have the advantage as the uterus can be preserved especially in young women. However, none of the published cases utilized these techniques. Some of the patients have shown complete disappearance of the lesion at 6–12 months postpartum by imaging studies. But this is unknown whether this regression was the result of natural history of the lesion or lack of hormonal stimulation in the post-partum period. 12 It is usually not common to find cavernous haemangiomas in women who are not pregnant because majority of them are undiagnosed or are just lumped up as cases of menorrhagia in women with uterine fibroids, unlike in women who are pregnant and will present with significant antepartum, intrapartum or postpartum haemorrhage. [13]
CONCLUSION
This case underscores the importance of uterine cavernous haemangioma as one of the important differential diagnoses to be considered whenever a woman with diagnosed or undiagnosed uterine fibroids presents with significant menorrhagia. In addition, this case report indicates that this condition is probably not as uncommon as thought. This could have gone undiagnosed clinically as it almost happened in this index case. It is very important to subject all hysterectomy specimens for histopathological examination.
REFERENCES
- Insun K, Seung YH, Sang AY, Kyu WL. Arteriovenous Malformations of the Uterus - a Case of Massive Operative Bleeding. J Korean Med Sci 1991; 6:187-90
- Virk RK, Zhong J, Lu D. Diffuse Cavernous Hemangioma of the Uterus in a Pregnant Woman: Report of a Rare Case and Review of Literature. Arch Gynecol Obstet. 2009; 279:603-5 doi: 10.1007/s00404-008-0764-7
- Bhavsar T, Wurzel J, Duker N. Myometrial Cavernous Hemangioma with Pulmonary Thromboembolism in a Post-Partum Woman: A Case Report and Review of the Literature. J Med Case Rep. 2012; 6:397
- Benjamin MA, Yaakub HR, Telesinghe P, Kafeel G. A Rare Case of Abnormal Uterine Bleeding caused by Cavernous Hemangioma: A Case Report. J Med Case Reports 2010; 4:136 doi:10.1186/1752-1947-4-136
- Lotgering FK, Pijpers L, van Eijck J, Wallenburg HC. Pregnancy in a Patient with Diffuse Cavernous Hemangioma of the Uterus. Am J Obstet Gynecol 1989; 160:628-30 doi:10.1016/s0002-9378(89)80044-4
- Uotila J, Dastidar P, Martikainen P, Kirkinen P. Massive Multicystic Dilatation of the Uterine wall with Myometrial Venous Thrombosis during Pregnancy. Ultrasound Obstet Gynecol 2004; 24:461-3 doi:10.1002/uog.1702
- Chou WY, Chang HW. Uterine hemangioma: a rare pathologic entity. Arch Pathol Lab Med 2012; 136:567-71 doi: 10.5858/arpa.2011-0078-RS
- Sharma JB, Chanana C, Gupta SD, Kumar S, Roy K, Malhotra N. Cavernous Hemangiomatous Polyp: an unusual case of Perimenopausal Bleeding. Arch Gynecol Obstet. 2006 Jul;274(4):206-8. doi: 10.1007/s00404-006-0161-z. Epub 2006 May 18. PMID: 16708224.
- Majmudar B, Ghanee N, Horowitz IR, Graham D. Uterine Arteriovenous Malformation necessitating Hysterectomy with Bilateral Salpingo-oophorectomy in a Young Pregnant Patient. Arch Pathol Lab Med. 1998 Sep;122(9):842-5. PMID: 9740147.
- Johnson C, Reid-Nicholson M, Deligdisch L, Grinblat S, Natarajan S. Capillary Hemangioma of the Endometrium: A Case Report and Review of the Literature. Arch Pathol Lab Med. 2005 Oct;129(10):1326-9. doi: 10.5858/2005-129-1326-CHOTEA. PMID: 16196525.
- Sütterlin MW, Müller T, Rehn M, Rempen A, Dietl J. Successful Abdominal Delivery in a Woman with Sonographic Diagnosis of Diffuse Cavernous Hemangioma of the Uterus. Am J Perinatol. 1998;15(7):423–425. doi: 10.1055/s-2007-993969.
- Shanberge JN. Hemangioma of the Uterus Associated with Hereditary Hemorrhagic Telangiectasia. Obstet Gynecol. 1994 Oct;84(4 Pt 2):708-10. PMID: 9205458.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’s Soft Tissue Tumors. St Louis, MO: Mosby; 2001.