Corresponding:
Adebayo Babafemi Charles Daniyan
National Obstetric Fistula Centre, Abakaliki, Nigeria
abcdaniyan@gmail.com
+2348033803982
Introduction
Obstetric fistula remains a problem in Nigeria and other low- and middle income countries.1 It is an abnormal communication between the vagina and the bladder (vesicovaginal fistula) and/or the rectum (rectovaginal fistula) resulting in uncontrollable leakage of urine and/or faeces.2 It is a devastating condition that results from prolonged obstructed labour, Caesarean section, instrumental vaginal delivery, destructive vaginal delivery, and caesarean hysterectomy.3,4 The underlying predisposing factors include poverty, illiteracy, cultural practices, early marriage lack of access to quality maternity services such as emergency obstetric care.3,4The continuous leakage of urine and/or stool results in persistent odor with serious psychosocial and economic consequences such as shame, isolation from the society, rejection by the husband and family members, loss of status and dignity, loss of social and financial support, depression and suicidal ideation. 3
An estimated 2 million women and girls are said to be living with obstetric fistula globally with about 50,000–100,000 new cases occurring annually.4The burden is highest in developing countries especially the sub-Saharan Africa and South-East Asia. Nigeria contributes 40% of the global burden with approximately 12,000 new cases per year and 150,000 awaiting surgery.4 In 2008, the Nigeria demographic health survey put the prevalence of obstetric fistula at 0.3% in South-East Nigeria, a value lower than the average of 0.4% nationally. A prevalence of 4.3% was reported in Abakaliki.6 The unmet need for fistula repair has been estimated to be as high as 99%.14 Less than 5000 obstetric fistula patients are offered surgery yearly in Nigeria, at different levels of expertise.4 At this rate, it will take about 100 years to clear the backlog, ignoring the new cases.7
Surgery remains the mainstay of treatment, although conservative management has been employed for very small fistula via prolonged bladder catheterization or via injection of fibrin-based glue.8 Success rate after repair varies from center to center and is determined by many factors like the size and site of fistula, previous repairs, degree of vaginal scarring, repair technique, equipment, expertise, post-operative care among others. Success rate can be as high as 92%.9First repair offers the best chance of successful closure and repeat surgery for a failed repair cause additional economic and psychosocial burden to the woman and the care givers.10 Hence, it is important to identify factors associated with successful obstetric fistula repair for the purpose of counseling, preoperative preparation and development of checklists to improve the chances of a successful surgery. The study was carried out to determine the factors that predicts successful obstetric fistula repair at the National Obstetric Fistula Centre Abakaliki.
Methodology
Study Area
The study was conducted at the National Obstetric Fistula Centre (NOFIC), Abakaliki, Ebonyi state, South-East Nigeria. NOFIC is the national reference centre for the management of obstetric fistula in the southern part of Nigeria, serving the South-East, South-South, South-West and parts of the North-Central geo-political zones of the country. The Centre is located at 86km Enugu-Abakaliki Expressway and receives patientsfrom about 20 states of Nigeria, the Federal Capital Territory and neighboring Cameroun. The centre has carried over 3,000 free fistula repairs since inception.
Study Design
It was a prospective cohort study.
Study Duration
It was carried out over a period of 6 months from 1st August 2021 to 31st January 2022.
Study Population
The study population comprised obstetric fistula patients who had surgical repair at NOFICAbakaliki during the 6-month period.
Inclusion Criteria
- All new patients with obstetric fistula
- Obstetric fistula patients with previous failed repair
Exclusion Criteria
- Patients with fistula from non-obstetric cause
- Patients with obstetric fistula of less than 3 months duration
- Patients with uretero-vaginal fistulas
Sampling Technique
Consecutive sampling of all obstetric fistula patients who met the inclusion criteria was used to recruit patients for the study.
Data collection
The patients were counseled and written informed consent was obtained at recruitment. Detailed history was taken from the patients. Physical and pelvic examination in lithotomy position was performed to confirm the diagnosis. Fistula was classified using the Lawson’s classification. Fistula characteristics such as location, size, number, circumferential defect, presence or absence of vaginal fibrosis, previous repair and the urethral length were determined. Information on sociodemographic characteristics, fistula characteristics, operative findings, postoperative care and outcome of repair were entered into a structured questionnaire.
Data Analysis
Data obtained from this study was analyzed using the IBM Statistical Package for Social Sciences (SPSS) version 24.0 software. Descriptive analysis was performed using means, medians and standard deviations. Test of associations of sociodemographic, obstetric characteristics, fistula characteristics and perioperative factors with outcome of repair was done using Chi-square test and Fischer’s exact test. Association at P-value less than 0.05 was considered statistically significant.
Ethical Consideration
Approval for the study was obtained from the Research and Ethics Committee of NOFIC. Informed written consent was obtained from the subjects before enrollment. Participants were assured that all information would betreated confidentially and that they were free to decline from participation or withdrew from the study without any penalties.
Results
A total of 120 patients that met the inclusion criteria were recruited. The mean age of the women was 30.4±6.6 years.The mean duration of symptoms was 15.86+12.7 months. One hundred and seventeen women had vesico-vaginal fistula while 3 had both VVF and RVF. Of the 117 patients with vesico- vaginal fistula, intracervical fistula (55) was the commonest and vault fistula (4) was the least common. Fistula closed with continence was the outcome in 100 (83.4%) women. Fistula closed with residual incontinence was the outcome in 10 (8.3%) women, while failed repair was the outcome in 10 (8.3%) women. The patients’ age, parity, educational status, occupation, body mass index, place of delivery and antenatal status did not influence the outcome of repair.
Table 1: Effect of Patients’ Sociodemographics on Repair Outcomes

However, mode of delivery of antecedent pregnancy had influence on outcome of repair as patients who had Caesarean section had more successful repairs (98.5%) than those who had spontaneous vaginal delivery (63.2%) and instrumental vaginal delivery (54.5%). This was statistically significant (P=0.000).
Table 2: Effect of obstetric characteristics on repair outcome.

F = Fishers exact test. * = Significant at p<0.05
The presence of a live baby from the antecedent pregnancy was associated with a higher success rate post repair (91.5%) than those who had stillbirths (57.8%) and this was statistically significant (0.021). See Table 4b.
Table 5 shows that patients with duration of fistula of less than 6 months had a higher rate of successful repair (100%) as the success rate diminishes with increased duration as seen in patients who had fistula for more than 36 months (40%). This was statistically significant(P=0.000).
Fistula type, fistula size, vaginal scarring, urethral length and previous repair significantly affected the outcome on fistula repair. Patients with intracervical, juxtacervical, vault and vesico-uterine fistulae had a higher rate of successful repairs (100%) while fistulas with urethral involvement (circumferential and juxtaurethral fistulas) had lower rate of successful repairs (61.2%). All Patients with combined fistula (VVF & RVF) had failed repair (100%). This was significant (P=0.000).
Participants with small fistulas had more successful repair (100%) than those with large fistulae (62.1%) and this was statistically significant (P=0.001). Clients with moderate to severe vagina scarring Table 3 Effect of fistula characteristics on repair outcome.

* = Significant at p<0.05
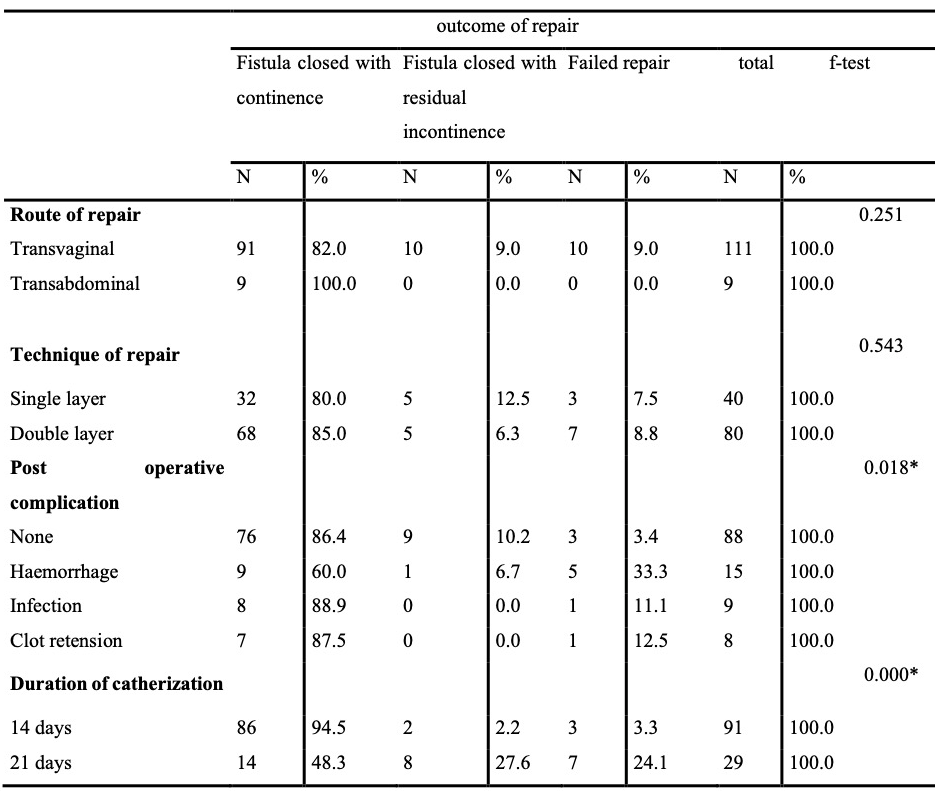
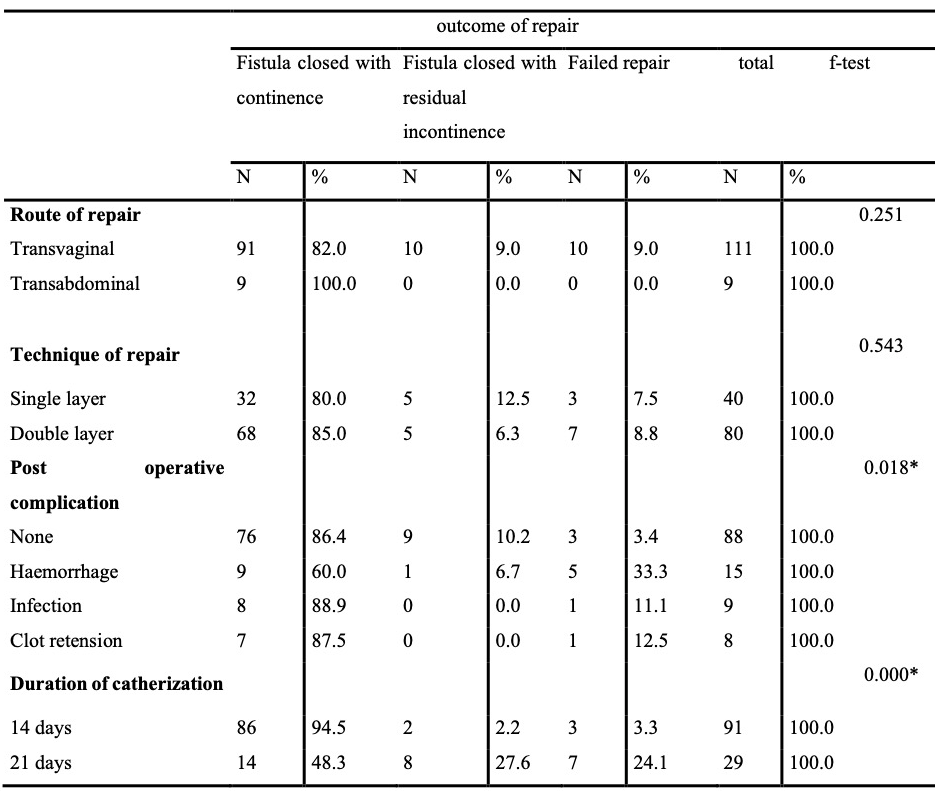
Table 4 Effect of periopertive care on repair outcome
F = fishers exact test. * = significant at p<0.05
were more likely to have failed repair (81.8% for severe) or residual incontinence (31.6% for moderate) than those with mild or no vaginal scarring. This was statistically significant (P=0.000).
Patients with no previous repairs had more successful repair (94.9%) than those with prior surgery. The success rate reduces as the number of previous unsuccessful repair increases as seen in patients with more than one previous repair (28.6%). This was statistically significant (P=0.000)
Participants with urethral length of 2 cm and above after repair had more successful outcome (90.5%) than those with urethral length of less than 2 cm (8.3%). Failed repair (50%) and residual incontinence (41.7%) was seen in those with urethral length of less than 2 cm(P=0.000).
Table 4 shows the route of repair does not seem to have much influence on the outcome of repair. Patients who had trans-vaginal repair had success rate of 82%. Success rate for those that had trans-abdominal repair was 100%, although less patients were repaired via this route. This was not statistically significant (P=0.251). Also, number of layers of closure, whether single or double, did not influence the outcome of repair as this was statistically not significant (P=0.543).
Participants who had no complications during the post-operative period had more successful repairs (86.4%). Failed repair was seen in patients who had haemorrhage (33.3%), infections (11.1%) and clot retention (12.5%) as the post-operative complications. This was significant (P=0.018). Those who had catheter for 14 days had successful repairs (94.5%) compared with those who had catheter for 21 days (43.3%).
Discussion
The mean age of the patients was 30.4+6.6 years, which was similar to that reported by Morhason-Bello et al11 but more than 25 years reported by Barone et al12. This is because in Barone et al, the study was a multinational multicenter study involving most of the West African countries where early marriage is being practiced. Also centres from Nigeria that were included in the study was from the northern part of the country where early marriage was common.
Majority of the patients had a vesico-vaginal fistula while few had both vesico-vaginal fistula and recto-vaginal fistula. This compares to studies by Barone et al12 and Kayondo et al13where most patients had vesico-vaginal fistula. This high number of vesico-vaginal fistula compared to rectovaginal fistula is probably due to the increased likelihood of compression anterior vaginal wall and the bladder by the fetal head against the bony pelvis hence causing more ischemia to the bladder than the rectum.
In this study, the success rate was 83.4%. This is similar to the study by Barone et al12 where the success rate was 84.5%, but less than that in a study from Jos9 where the success rate was as high as 92%. In this study, outcome of repair was determined at discharge when healing was not yet complete. It is possible for some women who were discharged with fistula not closed to be dry after some months. It is also possible that some with residual incontinence may eventually improve with physiotherapy in the long term. Also, some women who were discharged dry and continent may come back leaking from residual fistula at 3 months follow-up visit. Outcome of repair may be better determined at 3 months but many women who had closed fistula with continence may not return for follow-up. As seen from this study, the success rate is dependent on multiplicity of factors.
Age does not seem to have an influence on outcome of repair as seen in this study as opposed tothe study done in UCH, Ibadan11 where younger women aged 20-39 years had more successful outcome than women greater than 40 years. The reason why the study from UCH attributed more success in younger age group was because they tend to have better tissue healing process than in older group. Also, parity has no influence in this study in predicting treatment outcomes. Similar findings were reported in other studies done by Browning14 and Kirschner15.
Patients who had caesarean delivery had a higher rate of successful repairs than those who had spontaneous vaginal delivery. More failed repairs were seen those who had vaginal delivery. These findings are similar to study done in Guinea16 where spontaneous vaginal delivery was associated with increased failed repair and residual incontinence. This is because patients who had spontaneous vaginal delivery following prolonged obstructed labour could have more genital trauma resulting to extensive injury, more tissue loss and increased fibrosis than those who had caesarean delivery with a focal injury on the bladder. Also, urethral involvement is more likely in vaginal delivery than Caesarean section.
The presence of a live baby despite having a fistula is associated with a higher success rate post repair (91.5%) as against those who lost their babies and develop fistula (57.8%). This is because live babies in fistula patients are more common following Caesarean delivery and fistulas from caesarean section are usually distant from the urethra with less injury, tissue loss and fibrosis.
Patients treated within 6 months of having fistula had a higher success rate (100%) and less persisting incontinence than those women who were treated after 12 months (80.4%) after development of fistula and the success rate reduced as the duration of fistula increases. This is similar to study done in DRC17 where those treated within 6 months had a success rate of 92.4% than those treated after 12 months (84.3%). The possible explanation could be that fistula that is less than 6 months may have tissues around it that may be less scarred, healthy and readily mobile, with adequate blood supply which may enhance good healing after repair. However, as the duration of the fistula is prolonged, the risk of fibrosis around the fistula is increased from recurrent infections or from the effect of chemical inflammation caused by corrosive substances inserted in the vagina in an attempt to cure the ailment. The study from DRC however showed that the duration of fistula is not an independent predictor of outcome as other factors are also important.17
Successful fistula repair outcome was significantly associated with fistula type, urethral involvement, fistula size, previous repair and level of vaginal scarring. Fistulas that are away from the closing mechanism or fistulas without urethral involvement tend to have a better outcome than those involving the closing mechanism or urethra. In this study, intracervical and juxtacervical fistulas had the highest rate of successful repairwhile juxtaurethral fistula had the lowest. This is comparable to findings by Morhason-Bello et al11 where patients with juxtacervical fistula recorded the most favorable outcome (85.7%) followed by midvaginal (79.2%) and, then juxtaurethral (50.0%). Patients with Juxtaurethral fistula accounted for 27.8% of closed fistula with residual incontinence while those with circumferential fistula accounted for 62.5% of failed repair. This is comparable with study done in western Uganda13 where patients with circumferential fistula are 9 times more likely to fail from repair and patients with juxtaurethral fistula are 10 times more likely to have incontinence after successful closure.
In this study, patients who had both VVF/RVF had failed repair despite repair done by experienced surgeons. Though, the combined fistulas were associated with extensive fibrosis from the effects of prior repairs and use of corrosive substances in the vagina which may have affected the outcome. Also combined fistulas are more likely to be associated with extensive tissue loss. However, a study by Morhason-Bello et al11 showed that some patients with combined fistula had a successful outcome while others had closed fistula with residual incontinence. The reason could be that the fistulas were not associated with severe fibrosis and patients have been operated upon for the first time.
Study by Browning18 found that as the fistula size increased, the likelihood of residual incontinence increased after having adjusted for other fistula and patient characteristics. In this study, fistula size less than 2 cm have a higher success rate than fistulas whose size was 4 cm and above. This was comparable with a study in DRC17 where fistula size greater than 4 cm is associated with failed repair. Another study by Dennis et al19also noticed fistula size has an influence on outcome, as fistula size > 3 cm was associated with 2.41fold higher odds of surgical failure compared to fistulae less than 3 cm. Increased size of fistula is associated with increased tissue loss and extensive dissection during repair with consequent healing by fibrosis. Scarring can often cause the urethra to be pulled open, removing the physiological function, hence resulting to residual incontinence. Failed repair may result from minimal tissues available to mobilize in closing the fistula.
Patients who had no prior repairs had a higher success rate than those who had 2 prior repairs. This is quite similar to a study by Solbjorg et al17 in DRC where patients with 3 or more prior repairs are 4.7 times more likely to fail or 2.8 times more likely to have residual incontinence. Repeated fistula repairs may increase tissue fibrosis, reduce vaginal capacity and increase the likelihood of urethral involvement, all of which are factors in failed repairs.
Vaginal route of repair has been associated with less blood loss, less infections, less morbidity and short hospital stay compared to the abdominal route. However, abdominal route is often considered to be most appropriate for complex fistulas with ureteric involvement, intracervical fistula, supra or infra trigonal fistula and repairs which require bladder augmentation or omental flaps for large fistula. In this study, most fistulas were repaired through the vaginal route. In this study, the route of repair did not have much influence on outcome as seen in similar studies by Morhason-Bello et al11 and Chigbu et al20 where both studies did not find any significant difference for successful repair outcome in both routes. Double versus single layer closure technique in this study, appeared not to affect outcome of repair as seen in a study by Browning.18
In this study, patients who had catheter in situ for 21 days tended to have more residual incontinence and failed repair as compared to patients who had catheter for 14 days. This is not in agreement with the RCT by Barone et al where 7 days versus 14 days post-operative bladder catheterization showed no significant difference in outcomes.12This may be because the RCT was for simple fistula unlike this study where complex fistulas were included. Patients placed on extended periods of catheterization beyond the traditional 14 days are usually those who already have failed repair and leaking despite the presence of urethral catheter.
Conclusion
The predictors of successful repair are Caesarean delivery, absence of urethral involvement, mild or no vaginal fibrosis, no previous repair, moderate size fistulas, urethral length greater than 2cm, catheterization for 2 weeks and uneventful post-operative period. Patient characteristics do not affect the outcome of repair. These factors should be taken into consideration during pre-operative counseling and preparation of patients to ensure patients are aware of factors that may affect the outcome of repair and to allow adequate preparations to be put in place.
Limitation
Outcome of repair was determined at discharge when healing was still ongoing, as against 3 months. Hence, some patients with successful closure but with residual incontinence may eventually improve with physiotherapy in the long term. Also, some women who were discharged dry and continent may come back leaking from residual fistula at 3 months follow-up visit.
Competing interests
The authors declare that they have no competing interests.
Source of funding: None
References
- Daniyan B. Obstetric fistula – an unceasing scourge in the developing world. J Neonatal Biol 2017; 6: 244. doi: 10.4172/2167-0897.1000244.
- Tebeu PM, Fomulu JN, Khaddaj S, Bernis LD, Delvaux T, Rochat CH. Risk factors for obstetric fistula: a clinical review. Int Urogynecol J 2012; 23: 387-94.
- Hancock B, Browning A. Practical Obstetric Fistula Surgery. London; Ashland, Ohio: Royal Society of Medicine Press; 2009: 1-180
- Federal Government of Nigeria. Federal Ministry of Health, Department of Family Health, Reproductive Health Division. National Strategic Framework for the elimination of obstetric Fistula in Nigeria, 2011–2015. 2012: 1–64
- Nigeria Demographic and Health Survey. 2008: 139–141.
- Sunday-Adeoye I,Patrick O, Ogbonnaya LU.Prevalence, profile and obstetric experience of fistula patients in abakaliki, southeast Nigeria.urogynecologia 2011;volume 25:e6
- Federal Government of Nigeria. Federal ministry of health, Department of family health, Reproductive health division. Standard of practice on obstetric fistula in Nigeria.2011:1-44.
- Harris N, Garthwaite M.vesicovaginal fistulae. Indian journal of urology.2010; 26:253-256.
- Lewis W.L, Karshima A.J, Kirschner C, Arrow smith S.D. The obstetric vesico-vaginal fistula: Characteristics of 899 patients from Jos, Nigeria. America Journal of Obstetrics and Gynaecology 2004; 190:1011-19.
- WHO 2014. Facts on obstetric fistula .Available at http://www.who.int/features/fact files /obstetric fistula /en/ Accessed February 21,2017
- Morhason-Bello IO, Ojengbede OA, Adedokun BO, Oladokun A,Okunlola A. Obstetric fistula repair in a Nigeria tertiary health institution; lessons learnt from the outcome of care.Trop J Obstet Gynecol 2011; 28: 122-128.
- Barone MA, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, Bello A et al: Determinants of postoperative outcomes of female genital fistula repair surgery. ObstetGynecol 2012; 120: 524– 531.
- Kayondo M, Wasswa S, Kabakyenga J,Nosmo M,Jude S, Amy S, et al. Predictor and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, Western Uganda. BMC Urology 2011; 11: 1–9.
- Browning A. Risk factors for developing residual urinary incontinence after obstetric fistula repair.BJOG. 2006; 113:482–5. [PubMed: 16489933]
- Kirschner C, Yost K, Du H, Karshima J, Arrow smith S, Wall L. Obstetric fistula: the ECWA Evangel VVF Center surgical experience from Jos, Nigeria. International Urogynecology Journal 2010; 21:1525–33. [PubMed: 20700729]
- Alexandre D, Theresa D, AbdoulHabib B, Abdoulaye T, Delphin K, Sidikiba S et al. Factors associated with obstetric fistula repair in Guinea: implication for practice. Reproductive 2016;13:135.
- Solbjorg S, Siri V, Denis M, Marthias O. Surgical outcome of obstetric fistula: a retrospective analysis of 595 patients.ACTA obstetrician et Gynecologica scandanavian.2011;753-760 r2016;13:135
- Browning A. Prevention of residual urinary incontinence following successful repair of obstetric vesico-vaginal fistula using a fibro-muscular sling. BJOG. 2004; 111:357–61. [PubMed 15008773]
- Denis M, Lisa P, Christine A, Alain M, Abigail R, Smith R, et al. Panzi score as parsimonious indicator of urogenital fistula severity derived from Goh and Waaldijk classification Int J Gynecol Obstetric 2018; 142:187-193.
- Chigbu CO, Nwogu-Ikojo EE, Onah HE, Iloabachie GC. Juxtacervical vesicovaginal fistulae: outcome by route of repair. J Obstet Gynaecol. 2006; 26:795–7. [PubMed: 17130034]