Spontaneous Mid-Term Uterine Rupture in a Woman with Previous Cornual Wedge Resection
Joshua E. Ifebude1, Oluseun O. Saanu1,2, Olayinka R. Kuboye1, Opeyemi A. Adedeji 1, Jamiu A. Ogunsola 1, Imran O. Morhason-Bello1,2
1Department of Obstetrics and Gynecology, University College Hospital,
Ibadan, Oyo State, Nigeria
2Faculty of Clinical Sciences, College of Medicine, University of Ibadan, Nigeria
Abstract
Uterine rupture is a potentially life-threatening fetomaternal condition. Although rare in the developed world, it remains a major cause of fetomaternal morbidity and mortality in the developing countries. The presented patient was a G2P0+1 woman on Highly active anti-retroviral therapy (HAART) with previous cornual wedge resection for cornual ectopic gestation who presented with lower abdominal pain and hypovolemic shock. Obstetric ultrasound done at presentation revealed features of uterine rupture. She had emergency exploratory laparotomy and repair of uterine rupture. Her post-operative period was uneventful and she was discharged on the 4th post-operative day. The clinical presentation of this rare case has demonstrated the significance of having a high index of suspicion for uterine rupture especially in women who have had a scarred uterus. Therefore, women who undergo cornual wedge resection should be counseled on the risk of uterine rupture in subsequent pregnancies and that these subsequent pregnancies should be booked in specialized centers with appropriate antenatal surveillance and care.
Introduction
Rupture of the pregnant uterus is a rare event that is associated with severe complications that could result in a near miss or maternal mortality as well as perinatal mortality. Ruptured uterus occurs when there is a disruption of the whole uterine muscle and the visceral peritoneum. It could occur due to blunt or sharp trauma, interventions that suddenly increase intrauterine pressure or cause frequent or uncontrolled uterine contraction or during manipulation of pregnant uterus.1,2
The incidence of uterine rupture is variable with a reported range of 0.3–1.7% for women with history of scarred uterus, and 0.03– 0.08% in women with an unscarred uterus.3 Most uterine rupture occur in women with previous uterine surgical scar from classical caesarean section, history of uterine rupture, myomectomy with disruption of endometrium or uterine perforation.4 Other risk factors associated with uterine rupture include grandmultiparity in labour, injudicious use of oxytocics during labour, uterine anomalies, internal podalic version with breech extraction, external cephalic version, instrumentation like forceps application or vacuum extraction and unsupervised vaginal delivery.5
Spontaneous rupture of an unscarred uterus is rarely reported in the literature relative to those that resulted from trauma or obstetric events.6] Uterine rupture is considered spontaneous if it occurs without contractile activity of the myometrium and not due to direct or indirect trauma to the abdomen such as domestic violence, accidents, and uterine manipulation.2,5 Spontaneous rupture may rarely occur in unscarred uteri with uterine infection, adenomyosis, uterine or placental anomalies, sacculation of the entrapped retroverted uterus and cephalopelvic disproportion or as a manifestation of an underlying connective tissue disease. 4,7–11 However, most cases of spontaneous uterine rupture are associated with a scarred uterus, usually due to prior caesarean section.12–14 Other predisposing factors include: previous dilatation and curettage, previous endometritis, previous pelvic radiotherapy, as well as previous uterine rupture.15–17
This is a case report of spontaneous uterine rupture in a nulliparous woman with previous wedge resection of a cornual ectopic pregnancy at gestational age of 16weeks and 2 days.
Case Presentation
Mrs AT, a known HIV positive 39year old gravida 2 para 0 + 1 woman that booked for antenatal care. She presented to the gynecological emergency unit, at a gestational age of 16weeks and 2 days, with complaints of lower abdominal pain and vomiting of 2 hours on the 31st of December, 2022.
The lower abdominal pain was sudden in onset, dull, aching, continuous, and initially localized to the suprapubic region but subsequently became generalized. The pain was rated with a score of 9/10 by the patient using the visual analog scale. There was no aggravating or relieving factor. The patient had two episodes of vomiting that contained recently ingested meals. There was associated generalized body weakness and progressive abdominal swelling.

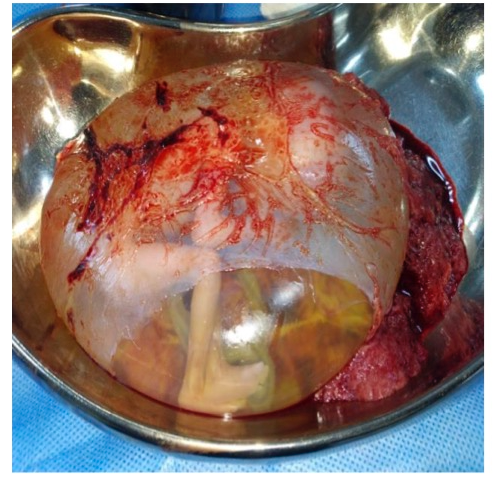
Figure 1: The right cornual rupture of uterus
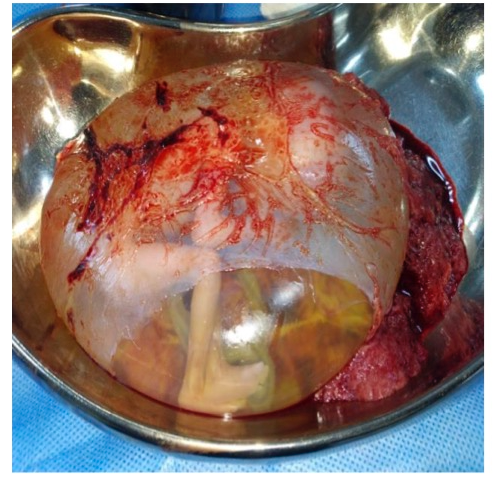
Figure 2: The abortus within the intact amniotic sac.
There was no history of abdominal trauma or history of fall or attempt at terminating her pregnancy. She had a pelvic ultrasound scan at gestational age of 6 weeks that confirmed intrauterine gestation and attended one antenatal clinic visit after booking and had no complaint. She was diagnosed with HIV in 2015 and was regular on highly active ante-retroviral drugs (Tenofovir, Lamivudine and Dolutegravir). Her latest viral load in February 2022 was 121copies/ml. There was past history of emergency laparotomy and right cornual wedge resection done on the 5th November, 2021, on account of ruptured right cornual ectopic pregnancy at gestational age of 10wks and 1day. In addition, a solitary pedunculated right cornual fibroid that measured 4cm X 3cm was removed. She did not have history of any other medical conditions.
The general physical examination showed a conscious and alert woman, in painful distress with conjunctival pallor. The pulse rate and blood pressure on admission were 108 beat/minute and 80/60mmHg, respectively, while the respiratory rate was 44 cycles per minute. The abdomen was distended, moved with respiration and there was generalized abdominal tenderness with guarding, it was difficult to palpate the intra-abdominal organs due to the abdominal tenderness. The vaginal examination revealed a closed cervix with minimal vaginal discharge. The bedside abdominopelvic ultrasound scan showed increased free intraperitoneal fluid in the peri-hepatic space, Morrison’s pouch, both para-colic gutters and pelvic cavity. An intrauterine fetus was seen within the uterus. However, a hypo-echoic line was seen extending from the placenta into the fundal myometrium suggestive of uterine rupture. The pack cell volume was 25%. A diagnosis of uterine rupture complicated with hypovolemic shock was made.
Resuscitation was commenced by infusing one liter of intravenous 0.9% normal saline fast and urethral catheter was passed to monitor urinary output. A written consent for emergency laparotomy was obtained after explaining the diagnosis and need for surgery to the patient. Under general anesthesia, the abdomen was cleaned and draped for laparotomy. A midline incision was made to gain access into abdominal cavity. The intra-operative findings include dense adhesions between the anterior abdominal wall, omentum, bowel and uterus; about 8cm linear rupture extending from the right cornual edge to the middle of the uterine fundus (Figure 1); about 4cm segment of the bowel was attached to the edge of the ruptured part of uterus; haemoperitoneum of 1.5 litres; and an intact gestational sac was extruded into the peritoneal cavity (Figure 2). The left fallopian tube was normal and both ovaries were seen and normal. The left tube was absent.
The foetus was extracted en-sac (Figure 1 & 2), the haemoperitoneum was suctioned, adhesiolysis was done and uterus repaired in two layers with polyglactin 910 no1 sutures. Hemostasis was secured. The patient was transfused with four units of cross-matched whole blood. The immediate post-operative management was uneventful, and her pack cell volume was 28%. She commenced fluid diets on the first postoperative day and solid diet on the second post-operative day. The findings at surgery and its implications, risk of uterine rupture in another pregnancy, the need for good health seeking behavior preferably at a tertiary Centre were explained to patient and her spouse, the discussion on contraception and future reproduction were also initiated. She was discharged home on the 4th postoperative day for follow-up at the gynecological clinic after two weeks
She was seen at the gynecological clinic follow-up visit; her wound had healed with primary intention. She was counseled again on the extent of surgery, the implications for future reproduction and the need for contraception to allow for adequate wound healing. The risk of uterine rupture in another pregnancy was discussed with the patient including encouraging the woman to register her future medical care at a tertiary health facility. She was referred to the family planning clinic and was discharged from the follow-up clinic.
Discussion
This is a rare case of spontaneous uterine rupture of a scarred uterus in second trimester that was promptly managed following a high index of suspicion and diagnosis. In some situation, the symptoms and signs may not be classical, and this could potentially delay diagnosis, treatment and sometimes fatality could occur.[18]
The patient presented with some classical symptoms that necessitated further investigations to clinch the diagnosis. It is important to counsel women who are at risk of spontaneous rupture to promptly present whenever they suspect any related symptoms such as sudden onset abdominal pain, new onset vomiting with or without bleeding per vagina as seen in the index case. The risk of scar rupture during a subsequent pregnancy is strongly related to the location of the previous scar, with upper uterine scars tending to rupture more easily and more often prior to the onset of labour than lower uterine segment scars12,13,19 . This patient had scar rupture in the fundus of the uterus at the site of previous cornual ectopic pregnancy that was resected and the uterus repaired. The increased susceptibility of fundal uterine rupture may be attributable to the attenuation of uterine musculature, poor connective tissue at the site of repair, a deficiency in the reconstruction of the uterine wall or tissue damage due to electro-surgery especially for laparoscopic procedures.8,15 Report from studies have shown that uterine rupture following cornual resection cannot be predicted or prevented and data on the absolute risk of uterine rupture is still unknown.20,21
It is recommended that women with scarred uterus secondary to cornual resection must be counseled on the risk of uterine rupture in subsequent pregnancy and advised on the warning symptoms and signs as well as the benefit of antenatal surveillance and care22 Symptoms of uterine rupture may range from severe (abnormal fetal heart rate, abdominal pain, bleeding, hypovolemic shock) to subtle and non-specific features like vomiting and generalized body weakness as seen our patient.15 Some cases of uterine scar rupture may be asymptomatic and are only detected incidentally at caesarean section. The most common ultrasound feature of uterine rupture is evidence of herniation of membranes through uterine defect.22 It is possible to visualize herniation of fetal parts – fetal limbs or umbilical cord – through the ruptured portion of previous wedge resection scar on ultrasound.8 However, this membrane could rupture resulting into leakage of fluid and haemoperitoneum23–25 . Our patient had evidence of uterine scar rupture on ultrasound and haemoperitoneum. In patients presenting late, there may be an empty uterus, expulsion of fetus and placenta from uterine cavity and absence of fetal heart activity.[23,26] Serial scans of cornual scar region with measurement of scar thickness has been suggested to predict the presence of scar dehiscence4,8,15, although there is no agreed standardized cut-off values similar to the evaluation of lower segment scar measurement.27 An emergency scan prompted by clinical symptoms in the index case enabled recognition of the defect in the cornual wedge resection scar site on the uterine fundus. A high index of suspicion of uterine scar rupture after eliciting a history of previous wedge resection helped the team to quickly make diagnosis after ultrasound and an urgent laparotomy was done for the patient.
This patient had uterine repair at laparotomy. The other management options include uterine repair with bilateral tubal ligation and hysterectomy. We repaired the uterus in this patient because she was nulliparous and desirous of pregnancy in the future. Another reason for our surgical decision is because the patient had healthy looking left fallopian tube. She was therefore counseled to register at a specialized health facility, register for antenatal care after her first missed period and present early for any ominous sign that is suggestive of a repeat episode of her complaint.
The role of HIV infection in patients on anti-retroviral therapy as it affects process of wound healing is not clearly defined in literatures.28–32 The contribution of HIV to poor wound healing and subsequent weakness leading to uterine rupture in this case cannot be substantiated. Therefore, further studies are required.
In conclusion, we reported a rare case of spontaneous uterine scar rupture in a woman that previously had cornual wedge resection for cornual ectopic gestation. We highlighted the importance of high index of clinical suspicion and role of ultrasound to make prompt diagnosis and institute emergency management.
References
- Cecchini F, Tassi A, Londero AP, Baccarini G, Driul L, Xodo S. First trimester uterine rupture. Int J Environ Res Public Health 2020;17(8):1–13.
- Ofir K, Sheiner E, Levy A, Katz M, Mazor M. Uterine rupture: Differences between a scarred and an unscarred uterus. Am J Obstet Gynecol 2004;191(2):425–9.
- Baskett TF, O’Connell CM. Severe obstetric maternal morbidity: A 15-year population-based study. J Obstet Gynaecol (Lahore) 2005;25(1):7–9.
- Hlibczuk V. Spontaneous uterine rupture as an unusual cause of abdominal pain in the early second trimester of pregnancy. J Emerg Med 2004;27(2):143–5.
- You SH, Chang YL, Yen CF. Rupture of the scarred and unscarred gravid uterus: Outcomes and risk factors analysis. Taiwan J Obstet Gynecol [Internet] 2018;57(2):248–54. Available from: https://doi.org/10.1016/j.tjog.2018.02.014
- Amro B, Lotfi G. Spontaneous rupture of an unscarred uterus in early pregnancy: A rare but life-Threatening emergency. BMJ Case Rep 2019;12(5):2018–9.
- Vimercati A, Dellino M, Suma C, Damiani GR, Malvasi A, Cazzato G, et al. Spontaneous Uterine Rupture and Adenomyosis, a Rare but Possible Correlation: Case Report and Literature Review. Diagnostics 2022;12(7):1–8.
- Nishijima Y, Suzuki T, Kashiwagi H, Narita A, Kanno H, Hayashi M, et al. Uterine rupture at 26 weeks of pregnancy following laparoscopic salpingectomy with resection of the interstitial portion: A case report. Tokai J Exp Clin Med 2014;39(4):169–71.
- Hawkins L, Robertson D, Frecker H, Berger H, Satkunaratnam A. Spontaneous uterine rupture and surgical repair at 21 weeks gestation with progression to live birth: A case report. BMC Pregnancy Childbirth 2018;18(1):1–5.
- Hou JH, Lee TH, Wang SY, Lai HC, Mao SP. Spontaneous uterine rupture at a non-cesarean section scar site caused by placenta percreta in the early second trimester of gestation: A case report. Taiwan J Obstet Gynecol [Internet] 2021;60(4):784–6. Available from: https://doi.org/10.1016/j.tjog.2021.05.037
- Masia F, Zoric L, Ripart-Neveu S, Marès P, Ripart J. Spontaneous uterine rupture at 14 weeks gestation during a pregnancy consecutive to an oocyte donation in a woman with Turner’s syndrome. Anaesth Crit Care Pain Med 2015;34(2):101–3.
- Moramarco V, Korale Liyanage S, Ninan K, Mukerji A, McDonald SD. Classical Cesarean: What Are the Maternal and Infant Risks Compared With Low Transverse Cesarean in Preterm Birth, and Subsequent Uterine Rupture? A Systematic Review and Meta-analysis. J Obstet Gynaecol Canada [Internet] 2020;42(2):179-197.e3. Available from: https://doi.org/10.1016/j.jogc.2019.02.015
- Endres LK, Barnhart K. Spontaneous second trimester uterine rupture after classical cesarean. Obstet Gynecol 2000;96(5 SUPPL.):806–8.
- Kanao S, Fukuda A, Fukuda H, Miyamoto M, Marumoto E, Furuya K, et al. Spontaneous Uterine Rupture at 15 Weeks’ Gestation in a Patient with a History of Cesarean Delivery after Removal of Shirodkar Cerclage. Am J Perinatol Reports 2013;4(01):001–4.
- Inovay J, Marton T, Urbancsek J, Kadár Z, Altdorfer K, Papp Z. Spontaneous bilateral cornual uterine dehiscence early in the second trimester after bilateral laparoscopic salpingectomy and in-vitro fertilization. Hum Reprod 1999;14(10):2471–3.
- Singhal SR, Gupta A, Nanda S. Spontaneous asymptomatic uterine scar dehiscence at 20 weeks of gestation as a result of endomyometritis. Arch Gynecol Obstet 2009;280(4):689–90.
- Huarte Ciganda M, Estaún Echavarren C, García Jiménez A, Huarte Sala I. Spontaneous Uterine Rupture in the Second Trimester in a Patient With Previous Pelvic Radiotherapy in Childhood: A Case Report. J Obstet Gynaecol Canada 2020;42(1):84–7.
- Maymon R, Mor M, Betser M, Kugler N, Vaknin Z, Pekar-Zlotin M, et al. Second-trimester and early third-trimester spontaneous uterine rupture: A 32-year single-center survey. Birth 2021;48(1):61–5.
- Bharatnur S, Hebbar S, Shyamala G. Early second trimester uterine scar rupture. BMJ Case Rep 2013;10–1.
- Brandt CA, Larsen B. Uterine Rupture after Re‐Implantation of Fallopian Tubes. Acta Obstet Gynecol Scand 1989;68(3):281–2.
- Stanirowski PJ, Trojanowski S, Słomka A, Cendrowski K, Sawicki W. Spontaneous Rupture of the Pregnant Uterus following Salpingectomy: A Literature Review. Gynecol Obstet Invest 2015;80(2):73–7.
- Tong C, Gong L, Wei Y, Liu Z, Wang Y, Yuan P. Ultrasonic diagnosis of asymptomatic rupture of uterine in second trimester of pregnancy after laparoscopic surgery for interstitial pregnancy: a case report. BMC Pregnancy Childbirth 2021;21(1):1–4.
- Ibrahim S, Drymiotou S, Hegab K, Sideris M, Okba M. Second trimester rupture uterus, unusual presentation. Ann Med Surg [Internet] 2021;61(October 2020):145–7. Available from: https://doi.org/10.1016/j.amsu.2020.12.020
- Ulkumen BA, Pala HG, Baytur Y. Acute abdomen and massive hemorrhage due to placenta percreta leading to spontaneous uterine rupture in the second trimester. Saudi Med J 2014;35(9):1131–2.
- Wininger, Fred A. , Zeng R., Johnson, G.S., Katz, M.L., Johson G.C., Bush, W.W. , Jarboe, J.M., Coates JR. Case report : Case report. Can Fam Physician 2020;47(10):788–9.
- Goynumer G, Teksen A, Durukan B, Wetherilt L. Spontaneous uterine rupture during a second trimester pregnancy with a history of laparoscopic myomectomy. J Obstet Gynaecol Res 2009;35(6):1132–5.
- Wye D, Magotti R, Al-Mashat D, Benzie R, Condous G. Sonographic diagnosis of spontaneous uterine rupture at the site of cornual wedge resection scar - a case report. Australas J Ultrasound Med 2014;17(1):45–8.
- Watts DH, Balasubramanian R, Maupin RT, Delke I, Dorenbaum A, Fiore S, et al. Maternal toxicity and pregnancy complications in human immunodeficiency virus-infected women receiving antiretroviral therapy: PACTG 316. Am J Obstet Gynecol 2004;190(2):506–16.
- Louis J, Landon MB, Gersnoviez RJ, Leveno KJ, Spong CY, Rouse DJ, et al. Perioperative morbidity and mortality among human immunodeficiency virus-infected women undergoing cesarean delivery. Obstet Gynecol 2007;110(2 I):385–90.
- Zhao CS, Li X, Zhang Q, Sun S, Zhao RG, Cai J. Early outcomes of primary total hip arthroplasty for osteonecrosis of the femoral head in patients with human immunodeficiency virus in China. Chin Med J (Engl) 2015;128(15):2059–64.
- Rodriguez-Garcia M, Patel M V., Shen Z, Bodwell J, Rossoll RM, Wira CR. Tenofovir Inhibits Wound Healing of Epithelial Cells and Fibroblasts from the Upper and Lower Human Female Reproductive Tract. Sci Rep [Internet] 2017;8(April):1–13. Available from: http://dx.doi.org/10.1038/srep45725
- Howard NE, Phaff M, Aird J, Wicks L, Rollinson P. Does human immunodeficiency virus status affect early wound healing in open surgically stabilised tibial fractures? A prospective study. Bone Jt J 2013;95 B(12):1703–7.