`

![]()
Umbilical Artery Doppler Velocimetry as a Predictor of Perinatal Outcome Among Antenatal Women with High-Risk Pregnancies
Alada SJ*1, Nyango DD2, Kahansim ML2, Goshit SJ2, Daru PH1
1 Department of Obstetrics and Gynaecology, Jos University Teaching hospital; 2 Feto-maternal Unit, Department of Obstetrics and Gynaecology, Jos University Teaching hospital.
* Corresponding Author
Phone no. +2348036775526
Email-sarah.alada@gmail.com
Abstract
Background: Perinatal morbidity is a huge burden globally, with greater impact in the developing countries. Umbilical artery Doppler velocimetry as an antenatal surveillance tool significantly reduces perinatal morbidity and mortality among high-risk pregnancies, especially those complicated with IUGR. Objective: To determine the association between abnormal umbilical artery Doppler velocimetry and perinatal outcome in high-risk pregnancies. Design: It was a hospital based prospective cohort study. Methodology: The study participants were 161 consenting pregnant women with high-risk pregnancies between 28 weeks and 38 weeks of gestation admitted into the antenatal ward of Jos University Teaching Hospital between 1st February, 2021 and 31st January, 2022. Data on socio demographic characteristics, obstetric history, gestational age, LMP, previous history of contraceptive use, irregular menstrual periods, and co-morbidities were obtained. Ultrasound scan was performed using a 3.5MHz convex probe of GE Voluson P8 4D ultrasound machine. The fetal biometric parameters were measured in 2D mode before the Doppler mode was activated for the velocimetry of the umbilical artery. Reduced end diastolic flow was measured as raised pulsatility index (PI) and resistive index (RI) above the 95th percentile. This procedure was repeated two weekly or more frequently depending on the abnormality noted. They were then followed up till delivery to determine the fetal outcome. Analysis was done using SPSS software version 20. Results: The prevalence of high-risk pregnancy was 41.2%. Hypertensive disorders accounted for 53.4% (86) of the study participants. Abnormal umbilical artery waveform pattern was found in 17.4%. The prevalence of IUGR among the study population was 14.9% (24). There were 95.7% (154) live births and 7(4.3%) stillbirths. There was statistically significant association between abnormal umbilical artery velocimetry and IUGR, preterm delivery, stillbirth, low birth weight, low APGAR scores at 5th minute and need for SCBU admission. Conclusion: Umbilical artery Doppler study is a useful antenatal surveillance tool for women with high-risk pregnancies. It is significantly associated with perinatal outcomes like IUGR, Preterm delivery, stillbirth, low birth weight, low APGAR scores at 5th minute. The poorer the Doppler indices, the worst the perinatal outcome.
Key Words: Umbilical artery, Doppler velocimetry, High-risk pregnancy, Fetal Surveillance
Introduction
Perinatal morbidity and mortality is a huge burden globally1. About two-thirds of the global 2.6 million stillbirths occur mostly in developing countries.2,3 In Nigeria, a stillbirth rate of 71/ 1000 deliveries was reported in a Maternal and Perinatal Health Survey4. High-risk pregnancies accounted for approximately 20% of the global perinatal mortality.5In Nigeria, high-risk pregnancies account for about 50% of perinatal mortality.6 When a pregnancy is complicated by a factor or factors that compromise the outcome of the mother or baby or both are considered high-risk.7 Hypertensive disorders in pregnancy, which include chronic hypertension, gestational hypertension, preeclampsia and preeclampsia superimposed on chronic hypertension are the major cause of placental insufficiency. Other high-risk conditions include pregestational diabetes, chronic renal disease, sickle cell disease, and antiphospholipid syndrome.
Placental insufficiency is the common pathway for most of these high-risk pregnancies.8 Placental insufficiency cause nutritional and respiratory deficits leading to fetal growth restriction. Early-onset IUGR leads to vascular changes in the fetoplacental unit. The end-diastolic flow in the umbilical artery is of clinical importance as it reflects the status of the placental circulation. The end-diastolic flow shows a continuous increase throughout gestation as a result of the decline in the foetal-placental impedance. The decrease in impedance with advancing gestation is a direct result of an increase in the number of tertiary stem villi that takes place with placental maturation.9,10High-risk pregnancies affect either the number or obliterate the small muscular arteries in the tertiary stem villi of the placenta leading to increasing resistance. There is an inverse relationship between placental vascular resistance and end-diastolic flow. In other words, the end-diastolic flow decreases progressively with an increase in placental resistance as a result of the obliteration of these placental tertiary stems villi.11,12 These Doppler changes begin when villous damage is >30%.8 and progressively increase to the ominous absent or reversed end diastolic flow when over 70 % of placental tertiary villi are obstructed.13
The human fetus is an efficient physiologic oximeter machine. When it encounters unfavourable circumstances as a result of situations like placental insufficiency, it mobilizes a spectrum of adaptive/compensatory responses. With worsening symptoms, the compensatory response gives way to the decompensatory response. These adaptive responses can be detected by close antenatal fetal surveillance.
Antenatal fetal surveillance remains a major challenge in modern obstetrics. The current clinical standard is the use of a biophysical profile (BPP). The BPP is a dynamic test of fetal well-being that combines ultrasonographic evaluation and a non-stress test (NST) otherwise called antenatal cardiotocograph (CTG). It suffers from important limitations, the key of which is waiting for the impact of the insult on the fetus before intervention. In addition, the ultrasound scoring is flawed as it assigns equal scores to parameters of varying significance.14 Furthermore, when the decrease in fetal activity is acute, amniotic fluid volume may not decrease. Similarly, CTG has a low sensitivity and high specificity. In other words, it is very good at telling which fetuses are well, but are poor at identifying which ones are unwell. While tracing with good variability provides strong reassurance of good fetal oxygenation, abnormal tracings poorly correlate with fetal status and have a high false-positive rate. Again, the loss of fetal heart rate variability in itself, may not necessarily be an ominous observation but normal fetal physiologic adjustments to a number of medications, illicit substances, or simply behavioural state.2 In addition, CTG has high intra and inter-observer errors. Furthermore, reactivity is not expected in early IUGR (<30 weeks). While 80% of fetuses beyond 32 weeks have a reactive NST, the rate of reactivity is lower in IUGR fetuses since CNS maturation is delayed, but centrally regulated responses to hypoxia remain preserved.15 Therefore, non-stress testing must be considered a secondary test and should ideally not be used by itself for IUGR monitoring.14 Other subjective fetal surveillance methods still in use in many institutions in developing countries include clinical symphysio-fundal height measurement and fetal heart rate monitoring, Cardiff and Sadovsky fetal kick count which relies on maternal perception of fetal movement, serial measurement of biometric parameters using a 2D ultrasound scan.2
Current evidence shows that umbilical artery Doppler velocimetry is a superior surveillance tool for predicting perinatal outcomes in high-risk pregnancies particularly those complicated by fetal growth restriction.17-20 It reduces the risk of perinatal death by approximately one-third, without increasing interventions such as iatrogenic preterm delivery.21 In addition, it is the clinical standard for distinguishing between SGA and IUGR, as well as for the clinical staging of IUGR. 22 Umbilical artery Doppler (UmAD) velocimetry assessment can be both qualitative and quantitative. Qualitatively, it can be described as reduced end diastolic flow, absent end diastolic flow (AEDF) or reversed end diastolic flow (REDF). Although there are other quantitative indices, the systolic to diastolic ratio (S/D), resistive index (RI) and pulsatility index (PI) represent those most commonly used. Absent and reversed end diastolic flow (AREDF) which represents an extreme abnormality in a waveform, is the only measure that provides both diagnostic and prognostic information for the management of IUGR. While AEDF is associated with an 80-fold increase in perinatal mortality, the presence of REDF has been related to a higher incidence of long-term permanent neurologic damage compared to IUGR fetuses with positive EDF. 23 In the same vein, research shows that in IUGR, the degree of neurodevelopmental abnormality in childhood is proportionally related to the impedance within the umbilical artery Doppler velocimetry.24 It is worth noting that only in pregnancies with suspected FGR does the use of umbilical artery Doppler sonography reduce the number of perinatal deaths and unnecessary obstetric interventions,25 as routine use of umbilical artery Doppler in low-risk pregnancies had shown no benefits.18
Despite the emerging evidence showing umbilical artery Doppler velocimetry as a superior surveillance tool in reducing perinatal morbidity and mortality in high-risk pregnancies, this benefit is yet to be fully maximized in our environment. This study aims to assess the use of umbilical artery Doppler velocimetry as a predictor of perinatal outcome among antenatal women with high-risk pregnancies in Jos University Teaching Hospital.
Methods and Materials
The study was conducted in the feto-maternal unit of the Department of Obstetrics and Gynaecology of Jos University Teaching Hospital over a period of one year from 1st February 2021 to 31st January 2022. It was a Hospital based prospective cohort study. The participants were one hundred and sixty-one (161) antenatal women with high-risk pregnancies between 28 weeks and 38 weeks of gestation. Participants who met the inclusion criteria were recruited from either the antenatal clinic or the antenatal ward. Inclusion criteria include Pre-existing medical disorders like pre-gestational diabetes, Chronic Hypertension, Renal disease, Sickle cell disease, previous history of IUFD / stillbirth and previous history of recurrent pregnancy losses. Exclusion criteria include women with multiple gestation, congenital anomaly of the fetus, unreliable follow-up, and high-risk pregnant women who did not consent to the study. A convenience sampling method was used, and an interviewer-administered semi-structured questionnaire was used to obtain data on socio-demographic characteristics, obstetric history, gestational age, LMP, previous history of contraceptive use, irregular menstrual periods, and co-morbidities. Ultrasound scan results were also obtained. The ultrasound scan was done by the investigator using a GE Voluson P8 4D ultrasound machine. A 3.5MHz convex probe was selected for both fetal biometric parameters which were measured in 2D mode before the colour flow mapping was activated to identify the vessel and define the direction of blood flow followed by the pulse wave Doppler velocimetry of the umbilical artery was performed at the free loop as the site of insonation. The accuracy of Doppler measurements was optimized according to the International Society of Ultrasound in Obstetrics and Gynaecology (ISUOG) Practice Guidelines: use of Doppler ultrasonography in obstetrics.26 A minimum of three waveforms in the original upright position were obtained. We ensure the correct position by watching the 2D image and also listening to the audible representation of the Doppler shift over the loudspeaker. The gain was adjusted in order to see clearly the Doppler velocity waveform.
Fetuses with EFW below the 10th percentile for their GA were adjudged SGA, while those SGA with abnormal umbilical Doppler, in addition, were tagged growth restricted (IUGR). Reduced end diastolic flow was measured as raised pulsatility index (PI) and resistive index (PI) above the 95th percentile. This procedure was repeated two weekly or more frequently depending on the abnormality noted. They were then followed up till delivery to determine the fetal outcome. The findings of the Doppler velocimetry were reported to the managing team if any abnormality was detected. Management of those with abnormal velocimetry followed the management protocol of attending Consultants. They were admitted for further evaluation and decisions were taken on timing and mode of delivery. Termination of the pregnancy was considered in the presence of any of the following: absence or reversal of end-diastolic flow in the umbilical artery, a non-reassuring test of fetal wellbeing (biophysical profile) and worsening maternal condition. Fetal/neonatal outcomes (gestational age at delivery, birth weight, live birth or stillbirth, Apgar score at 5 minutes, SCBU admission) were assessed after delivery. Analysis of the data was done using SPSS software version 20. Ethical approval was obtained from the ethical committee of the Jos University Teaching Hospital.
Results
A total of 2,506 pregnant women booked for antenatal care at JUTH during the study period out of which 1,032 were high-risk pregnancies giving a 41.2% prevalence for high-risk pregnancies. Table 1 shows the demographic characteristics. The mean age of the participants was 31.6 ± 5.8 years with an age range of 20-45 years. The majority 48(29.8%) were in the age range of 35-39 years. Ethnic distribution showed 61(37.9%) of the participants were Hausa while 58(36.0%) were Plateau Indigenous tribes, Yoruba 13 (8.1%) and Igbos 5 (3.1%). The study further revealed that 60(37.3%) of the participants were housewives and 74(46.0%) had a tertiary level of education.
Table 1: Maternal Demographic Characteristics (n = 161)

Table 2: Maternal Reproductive History (n = 161)

Table 2 shows the maternal reproductive history. Primigravidas were 28(17.4%), while 24(14.9%) were grandmultiparous. The average gravidity in this study was 4.1±2.7 pregnancies and the mean parity was 2.3±2.1 births. The majority of the participants (91.3%) had 0-4 living children while only 14(8.7%) had 5 and above living children. All the participants were booked for antenatal care. The average gestational age at booking was 17.4±6.4 weeks with 102(63.4%) booking at gestational age below 20 weeks.
Figure 1 shows the distribution of risk factors. Overall, hypertensive disorder in pregnancy was the commonest risk 86 (53.4%) with Chronic hypertension being 40(24.8%), PIH 28 (17.4%), preeclampsia 13 (8.1%), and chronic hypertension with superimposed pre-eclampsia 5 (3.1%). Previous IUFD was 36(22.4%).
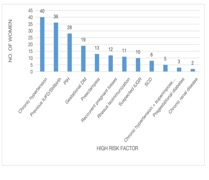
Figure 1: Risk for High-Risk Pregnancy
Table 3 Showing umbilical artery Doppler waveform pattern and indices

The prevalence of IUGR among the study population was 24 (14.9%). Table 3 shows the umbilical artery Doppler waveform pattern and indices. Normal umbilical artery waveform pattern was seen in the majority 111(68.9%) of the study group. The prevalence of abnormal umbilical artery waveform patterns in this study group was 17.4 % (n=28). Fourteen (8.7 %), 11 (6.9%), 2 (1.2%) and 1 (0.6%) participants demonstrated high RI, high PI, AEDF and REDF values respectively.
Table 4 shows the association between abnormal umbilical artery velocimetry and maternal/fetal outcome among women with high-risk pregnancies.
Table 4: Association between umbilical artery velocimetry (Doppler indices and waveform pattern) and Maternal/ fetal outcome among the study participants
(n= 161).

*Statistically significant f= Fisher’s exact test.
The majority 17(70.8%) of the fetuses with IUGR had abnormal umbilical artery velocimetry compared to 7(29.2%) who had normal umbilical artery velocimetry. This was statistically significant (p ≤ 0.0001). There was also a statistically significant association between abnormal umbilical artery velocimetry and gestational age at delivery (p = 0.008), Stillbirth (p = 0.002), birth weight (p ≤ 0.0001), APGAR score at 5th minutes (p = 0.001) and SCBU admission (p ≤ 0.0001). There was however no statistically significant association between abnormal umbilical velocimetry and mode of delivery, sex of the baby and early neonatal death.
Table 5 shows the relationship between the Doppler Waveform pattern and fetal outcomes. There was a statistically significant association between abnormal umbilical artery velocimetry and IUGR, preterm delivery, stillbirth, low birth weight, low APGAR scores at the 5th minute and need for SCBU admission.
Table 5: Relationship between Doppler Waveform Pattern and Fetal Outcome

f = Fisher’s Exact Test
* = Statistically Significant
ReDF = Reduced End Diastolic Flow (RI and PI), AEDF = Absent End Diastolic Flow, REDF = Reversed End Diastolic Flow
Discussion
The prevalence of high-risk pregnancy in this study was 41.2%. This was similar to the prevalence of 40.1% found in a study done in Enugu, Nigeria.6
It is however higher than the prevalence of 20% found in other studies.5,27 The higher prevalence in this study could be because our facility serves as a referral centre.
Most of the women in the study belong to the age range 35-39 years which is expected as advanced maternal age (35 years of age and older) is a known risk factor for most of the high-risk factors recruited in this study such as hypertensive disorders in pregnancy, gestational diabetes, recurrent miscarriages and IUGR. The majority of the women with high-risk pregnancies were multigravidas making up 82.6% of the study population which was similar to the study findings of Ahmed et al and Komuhangi et al.28 Hypertensive disorder in pregnancy was the commonest risk for high-risk pregnancy in this study which is similar to findings in other studies.29,30 This was not surprising as hypertensive disorders in pregnancy are the most common medical complications encountered in the developing world.30,31 The prevalence of abnormal umbilical artery velocimetry in this study was 17.4%. The prevalence of 1.8% for AEDF/REDF was similar to the prevalence of 2% for AEDF/REDF reported in a study in India.32 However, the overall prevalence of abnormal Doppler velocimetry was slightly higher than the previous study from Uganda where they reported a prevalence of abnormal flow pattern to be 10.95% with AEDF and REDF reported as 4.2% and 0.6% respectively.26 It was however lower than studies by Suryavanshi et al and Ahmed et al who reported a prevalence of 38.7% and 40% respectively. The difference could be a result of variations in the defined risk factors for high-risk pregnancy in the various studies.
There was a statistically significant association between abnormal umbilical artery Doppler velocimetry and preterm birth with 9(32.1%) out of 28 women with abnormal Doppler study delivering at gestational age less than 37 weeks compared to 16(12.0%) out of 117 women with normal Doppler findings. This was similar to findings documented in several previous studies.25, 33 Another significant observation in this study is that perinatal outcome is poorer in cases with abnormal umbilical artery Doppler velocimetry. Out of the 7 total number of stillbirths found in this study, 5(71.4%) had abnormal Doppler study compared to 2(28.6%) with normal Doppler study. Similarly, 71.4% of women with abnormal Doppler velocimetry had low birth weight babies (< 2.5kg) compared to 9.0% with normal Doppler study, 28.6% had babies with APGAR scores less than 7 at the 5th minute compared to 6.8% with normal Doppler study and 47.8% were admitted in SCBU compared to 10.7% with normal Doppler study. All these were statistically significant and in keeping with findings in similar studies by Alfervic et al, Komuhangi et al and Ahmed et al,.21, 28, 29 There was, however, no statistically significant association between mode of delivery and early neonatal death in this study which is in contrast with the findings in studies by Ahmed et al, Bhattacharjee et al and Suryavanshi among others.29, 30, 32
Factors such as extreme prematurity and unavailability of facilities to cater for such fetuses also tends to affect decision making to affect delivery in our environment. In addition, there is no defined protocol in our facility as regards the optimal timing of delivery during the management of such cases prompting the decision to conduct this study.
Absent end-diastolic flow (AEDF) and reversed end-diastolic flow (REDF) are generally associated with severe IUGR and a high incidence of overall perinatal mortality. In this study, absent end diastolic flow was associated with 100% perinatal mortality (IUFD).
A study by Brar et al reported 50% perinatal mortality in fetuses with reverse-end diastolic flow REDF.33 Similarly, Ahmed et al reported a perinatal mortality rate of 40% in the same group.30 This is supported by previous reports which show that Absent and reversed end diastolic flow (AREDF) which represents an extreme abnormality in the waveform is associated with an 80-fold increase in perinatal mortality, and the presence of REDF is associated with a higher incidence of long-term permanent neurologic damage compared to IUGR fetuses with positive EDF.23 Reduced end diastolic flow (high PI and RI) on the other hand had a better perinatal outcome with stillbirth occurring in only 2(10.5%) of cases. IUGR was however high in this group 14 (73.7%) with APGAR scores less than 7 at the 5th minute found in 5(26.3%), 7(58.8%) required SCBU admission and 2(11.7%) had early neonatal death. These findings were comparable to other documented studies.30, 33 This study was not without its own limitations. This was a single-centre prospective study done in Jos University teaching hospital and thus findings may not be generalized to the whole population of women with high-risk pregnancies in Jos or Nigeria. There is a need for a larger multicentre study.
Umbilical artery Doppler velocimetry is a valuable tool for fetal surveillance. Abnormal umbilical artery Doppler velocimetry is a common finding in women with high-risk pregnancies. AEDF and REDF are associated with 100% perinatal mortality. Its use in high-risk pregnancies particularly those complicated by utero-placental insufficiency will significantly improve obstetric decision making thereby reducing perinatal morbidity and mortality.
References
- World Health Organisation (WHO). WHO | Stillbirths [Internet]. Who. 2016. Available from: https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en,
- Pawar A, Damania K. Identification and Antepartum surveillance of High risk pregnancy. In: Bhide A, Arulkumaran S, Damania K, Daftary S, editors. Arias’ Practical guide to High Pregnancy and delivery: A South Asian perspective. 4th ed. Reed Elsevier India private Ltd; 2015. p. 116–34.
- World Health Organisation (WHO). WHO | Stillbirths [Internet]. Who. 2016. Available from: https://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en /.
- Fawole AO, Shah A, Tongo O, Dara K, El-Ladan AM, Umezulike AC, et al. Determinants of perinatal mortality in Nigeria. Int J Gynecol Obstet. 2011; 114: 37-42.
- Farajnezhad F, Shaahmadi F, Fashi Z, Daaylar L. Prevalence of high risk pregnancy and some relevant factors in referred women to health centers. J Sci Achiev. 2017; 12(2): 4-7.
- Aniebue UU, Aniebue PN. A risk assessment for pregnancy using the World Health Organization classifying form in primary health-care facilities in Enugu, Nigeria. Trop Doct. 2008; 38(3): 135-7.
- Coco L, Giannone TT, Zarbo G. Management of high-risk pregnancy. Minerva Ginecologica. 2014.
- Baschat AA. Fetal growth restriction - From observation to intervention. Journal of Perinatal Medicine. 2010; 38: 239-46.
- Fleischer A, Schulman H, Farmakides G, et al: Umbilical artery waveforms and intrauterine growth retardation. Am J Obstet Gynecol 151:502, 1985.4.
- Ott WJ: The diagnosis of altered fetal growth. Obstet Gynecol Clin North Am 15:237, 1988.
- Giles WB, Trudinger BJ, Baird PJ: Fetal umbilical artery flow velocity waveforms and placental resistance: pathological correlation. Br J Obstet Gynecol 92:31, 1985.
- Ayyuba R, Abubakar I, Yakasai I. Umbilical artery Doppler velocimetry study on prediction of adverse pregnancy outcomes among pregnant women with hypertensive disorders in Kano, Nigeria. Niger J Basic Clin Sci. 2015; 12: 95-104.
- Fleischer A, Goldenstein R, Bruner J, Worrell J. Doppler Sonography in Obstetrics and Gynaecology. In: Callen P, editor. Ultrasonography in Obstetrics and gynaecology. 3rd ed. Philadelphia: WB Saunders; 1994. p. 503–23.
- Siristatidis C, Kassanos D, Salamalekis G, Creatsa M, Chrelias C, Creatsas G. Cardiotocography alone versus cardiotocography plus Doppler evaluation of the fetal middle cerebral and umbilical artery for intrapartum fetal monitoring: A Greek prospective controlled trial. J Matern Neonatal Med. 2012; 25(7): 1183-7.
- Pillai M, James D. Continuation of normal neurobehavioural development in fetuses with absent umbilical arterial end diastolic velocities. BJOG An Int J Obstet Gynaecol. 1991; 98: 277-281.
- Bamfo JEAK, Odibo AO. Diagnosis and management of fetal growth restriction. Journal of pregnancy. 2011: https://doi.org/10.1155/2011/640715.
- Westergaard HB, Langhoff-Roos J, Lingman G, Marsál K, Kreiner S. A critical appraisal of the use of umbilical artery Doppler ultrasound in high-risk pregnancies: Use of meta-analyses in evidence-based obstetrics. Ultrasound Obstet Gynecol. 2001; 17: 466-476. 18.
- Alfirevic Z, Stampalija T, Gyte GM. Fetal and umbilical Doppler ultrasound in normal pregnancy. In: Cochrane Database of Systematic Reviews. 2010 (8): CD001450.
- Maulik D, Mundy D, Heitmann E, Maulik D. Evidence-based approach to umbilical artery doppler fetal surveillance in high-risk pregnancies: An update. Clinical Obstetrics and Gynecology. 2010; 58:869.
- Divon MY. Fetal growth restriction: Diagnosis. UpToDate. 2015. 28. American College of Obstetricians. ACOG Practice bulletin no. 134: fetal growth restriction. Obstet Gynecol. 2013; 121(5): 1122-1133.
- Alfirevic Z, Neilson JP. Doppler ultrasound for fetal assessment in high risk pregnancies. Cochrane Database Syst Rev. 2010 (1): CD00073.
- Figueras F, Gratacos E. Stage-based approach to the management of fetal growth restriction. Prenatal diagnosis. 2014; 34: 655-9.
- Figueras F, Gratacos E. Update on the diagnosis and classification of fetal growth restriction and proposal of a stage-based management protocol. Fetal Diagn Ther. 2014; 36:86–98.
- Levine TA, Grunau RE, McAuliffe FM, Pinnamaneni RM, Foran A, Alderdice FA. Early childhood neurodevelopment after intrauterine growth restriction: A systematic review. Pediatrics. 2015; 135; 126-41.
- Reddy A, Malik R, Mehra S, Singh P, Ramachandran L. Correlation of Doppler studies at 34 weeks of gestation with perinatal outcome in high risk pregnancies. Int J Reprod Contraception, Obstet Gynecol. 2015;(November 2015):1894–9.
- Ultrasound Obstet Gynecol 2013; 41: 233–239. Published online in Wiley Online Library (wileyonlinelibrary.com). DOI: 10.1002/uog.12371.
- Jain S, Anand S, Aherwar R. High Risk scoring for prediction of pregnancy outcome: a prospective study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2014;3(3):516-23.
- Komuhangi P, Byanyima RK, Kiguli-Malwadde E, Nakisige C. Umbilical artery doppler flow patterns in high-risk pregnancy and foetal outcome in Mulago hospital. Case Reports Clin Med. 2013;02(09):554–61. Ahmed A, Sharma R, Lahkar P. Umblical Artery Doppler in High Risk Pregnacy. Sch J Appl Med Sci. 2017;5(7B):2603–6.
- Ahmed A, Sharma R, Lahkar P. Umblical Artery Doppler in High Risk Pregnacy. Sch J Appl Med Sci. 2017;5(7B):2603–6.
- Suryavanshi MR, Katakdhond SS. Efficacy of doppler velocimetry of the umbilical artery in the defined high-risk groups to determine the fetal outcome. Int J Reprod Contraception, Obstet Gynecol. 2019; 8(5): 1724-1732.
- Devi J, Kumar D, Shukla M, Jain3 PK. Doppler interrogation of fetoplacental circulation in hypertensive disorder of pregnancy and their perinatal outcomes. Int J Res Med Sci. 2017; 5: 2687-93.
- L. R, Bhattacharjee A. Umbilical artery Doppler indices in relation to fetal outcome in high-risk pregnancy. Int J Reprod Contraception, Obstet Gynecol. 2018;7(2):628.
- Brar HS, Lowrence PD. Reverse end diastolic flow velocity on umbilical artery velocimetry in hgih risk pregnancies: an ominious finding with adverse pregnancy outcome. Am J obstet Gynecol. 1988; 159:559-61.