An Incidental Finding of Spontaneous Bilateral Ectopic Pregnancy: A Case Report
*Oni Olaolu.O1, Ogunkuade Margaret.F1, Akinmoladun Janet.A2, Olayemi O1.
1Department of Obstetrician and Gynaecolgist, University College Hospital, Ibadan
2Department of Radiology, University College Hospital, Ibadan
Abstract
Ectopic pregnancy (EP) is defined as the implantation of a fertilized ovum outside the normal endometrial cavity. Bilateral ectopic pregnancy is rare and occurs in 1 out of every 200,000 spontaneous pregnancies. A diagnosis of bilateral EP is usually made intraoperatively in developing countries. This is a 36-year-old G3P2 (2 alive) lady with two previous caesarean section admitted via the emergency unit with clinical features in keeping with EP. Pelvic ultrasound showed only a left tubal gestation of gestational age of 7 weeks with an empty uterus and haemoperitoneum. Laparotomy revealed an incidental finding of right ruptured ampullary ectopic gestation and left intact tubal gestation with massive haemoperitoneum. Right and left salpingectomy were done, and patient recovered well. Bilateral EP is rare but exists, therefore thorough inspection of the pelvis must be done during evaluation and surgical interventions so as not to miss it and to reduce morbidity and mortality associated with it.
Keywords: Bilateral ectopic pregnancy, Morbidity, Laparotomy, Salpingectomy.
Corresponding author:
Dr Olaolu Olayinka Oni
Consultant Obstetrician and Gynaecolgist,
University College Hospital, Ibadan.
08062087527 olaoluoni43@yahoo.com
INTRODUCTION
Ectopic pregnancy (EP) has remained a leading cause of maternal morbidity and mortality especially in sub–Sharan Africa1. Ectopic pregnancy is the result of a flaw in human reproductive physiology that allows the conceptus to implant and mature outside the endometrial cavity. The classic triad of symptoms – amenorrhea, abdominal pain and vaginal bleeding- occur in 50% of cases1.Spontaneous bilateral tubal EP is a very rare type of EP, and the incidence is 1 in every 200.000 spontaneous pregnancies and 1 of every 725 to 1580 ectopic pregnancies2. Haemorrhage is a complication of ectopic pregnancy and accounted for 4 to 10% of all pregnancy related deaths however this could be more in a patient with bilateral tubal EP 2,3. The case we presented here described a young woman who had bilateral tubal EP and subsequently had bilateral salpingectomy.
CASE REPORT
Mrs E.B was a 36-year-old, Gravida 3 Para 2, 2 alive woman with two previous caesarean section presenting at the gynaecological emergency of the hospital on the 28th of June,2021 (LMP was 08/05/2021) with seven weeks of amenorrhea, bleeding per vaginum and lower abdominal pain of two days duration. Lower abdominal pain was sudden in onset, dull aching, located in the right iliac fossa which later became generalised with pain score of 7 over 10. There was no history of trauma. She had not been on any contraceptive. She had no history of use of any ovulation induction drug and no family history of twinning. Her previous menstrual cycles were regular thirty days with bleeding period of 3 days. She had a history of shoulder tip pain at presentation.
General examination revealed that she was pale, afebrile and dehydrated. The respiratory rate was 22/min, pulse rate was 90 beats/min, blood pressure was 100/60mmHg. There was generalized tenderness with guarding on abdominal palpation.
Fig. 1. Right Tubal Ectopic Gestation
Fig. 2. Left Tubal Ectopic Gestation
Pelvic examination showed blood-stained perineum, non-bulky uterus with bilateral adnexal tenderness, closed cervical os, full pouch of Douglas and positive cervical excitation tenderness. Her packed cell volume was 22%. A urine pregnancy test done was positive. Pelvic ultrasound done per abdomen revealed a left adnexal gestation with cardiac activity in keeping with GA of 7wks and 1 day with an empty uterus and massive haemoperitoneum. A diagnosis of ectopic pregnancy with haemoperitoneum was made. Resuscitation was commenced while she was being worked up for laparotomy. Laparotomy revealed: dense pelvic adhesions involving the anterior abdominal wall with the rectus sheath and uterus with haemoperitoneum of 2000mls. These dense adhesions made the entry into the abdomen even through the midline difficult necessitating
Fig. 3. Histology Report
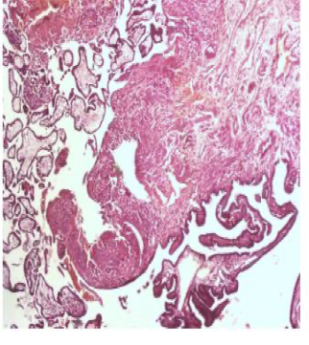

Fig. 4a Micrograph of left Fig. 4b Micrograph of
tubal gestation. right tubal gestation
sharp and blunt dissections of adhesives bands to assess the uterus and the adnexa. The right tubal ectopic gestation had completely ruptured at the ampullar region (Figure 1). The left tube contained an intact mass of ectopic gestation measuring 2 x 3 cm in the ampullar portion with a thinned out bulging point where it extruded intraoperatively (Figure 2), the remnant of the gestational sac was evacuated from the peritoneum with the clotted blood and sent for histology. The ovaries were partially buried in adhesions. Bilateral total salpingectomy was performed with drainage of haemoperitoneum. Total estimated blood loss was 2200ml. Patient had three units of blood transfused post operatively and she recovered well and was discharged on the 4th post-
operative day.
Histology of the specimens confirmed bilateral ectopic tubal pregnancy as shown in Fig 3, 4a and 4b (Photomicrographs). Informed consent was obtained from the patient to publish this report.
DISCUSSION
Spontaneous bilateral EP remains a rare type of extra uterine pregnancy. The incidence is 1 out of every 200,000 spontaneous pregnancies3. We present a case of incidental finding of spontaneous bilateral tubal pregnancy with a gestational sac on the left which ruptured intraoperatively and a ruptured right tubal pregnancy. Cases of spontaneous bilateral tubal pregnancy either ruptured or not ruptured have been reported earlier by Ghomian et.al and Njoku et.al 4,5. Most patients with bilateral EP have similar risk factors and symptoms as those with unilateral tubal ectopic pregnancy. The risk factors include tubal surgeries, prior caesarean sections (as in the case reported), assisted reproductive technology, prior abortion, pelvic inflammatory diseases etc. 6,7.
Diagnosis of EP is usually clinical though serum beta HCG assay and transvaginal ultrasonography (TVUS) have been found to be helpful. A case of preoperative diagnosis of bilateral EP according to ultrasonography findings was reported by Martinez et al unlike this reported case which was an incidental intraoperative finding8. However, sometimes TVUS might not reveal the bilateral EP. Andrews et al reported a case of spontaneous bilateral tubal pregnancy that a transvaginal pelvic ultrasound scan done only revealed an empty uterus with a unilateral (right) adnexal mass7 which was similar to the findings in this case reported.
Management options include expectant, medical and surgical9. In this case, a surgical option was chosen based on the haemodynamic stability of the patient and facilities available, however expectant management might be used for haemodynamically stable patient with unruptured ectopic pregnancy or those with no cardiac activity of the foetuses though this will be done as an inpatient in an hospital with 24-hour theatre facility and serial HCG assay with TVUS will be done to monitor the patient.
Management options of bilateral tubal pregnancy are many and the option to employ in each case depends on various factors which include, haemodynamic stability, presence of fetal cardiac activity, volume of haemoperitoneum, parity, desire for future pregnancy and available facility. The options ranges from bilateral salpingectomy as performed in this case to the conservative approach such as salpingostomy and salpingotomy7,10. A case report by Andrews et al on a patient with bilateral tubal pregnancy who had laparoscopic salpingectomy of the left tube and salpingotomy of the right tube has been documented7. The patient was subsequently treated with methotrexate because of persistent ectopic pregnancy. Since the diagnosis of bilateral tubal pregnancy is usually made at the time of surgery, there are no case reports of successful primary medical treatment with methotrexate11. Walter et al reported a case of bilateral chronic and acute tubal pregnancies where treatment with methotrexate failed12. When the exploratory laparotomy or laparoscopy is undertaken for ectopic pregnancy, inspection of both adnexa is necessary to determine the type of the surgery that will be needed (either radical or conservative) for nulliparous patient and in order not to miss a bilateral EP.
Follow up management following bilateral salpingectomy will depend on if the patient still desires to get pregnant. An option of assisted reproductive technique through in-vitro fertilization can be offered to patients who still desire pregnancy. Our patient has had two previous deliveries and had completed her family size and therefore needed no conservative surgery to preserve her fertility potential unlike the earlier mentioned bilateral EP cases.
CONCLUSION
Bilateral EP though rare, exists therefore both adnexa should be evaluated with TVUS to diagnose it pre-operatively, however this does not exclude a possibility of incidental finding of bilateral EP in laparotomy or laparoscopy as seen in this case. A high index of suspicion with TVUS might help early diagnosis and timely intervention which will help in preventing morbidity and mortality associated with this type of EP.
Source(s) of support: Self
Acknowledgement:
We sincerely appreciate the permission and consent given by the patient to publish the case report and the pathologist involved, Dr Ajani Mustapha who ensured the prompt histology results were available.
Conflicting Interest: None declared.
REFERENCES
- Igwegbe A.O, Eleje G.U, Okpala B.C. An appraisal of the management of ectopic pregnancy in a Nigerian tertiary institution. Obstet Gynae. 2013.
- Lawani O.L, Anozie O.B, Ezeonu PO. Ectopic pregnancy: a life threatening gynaecological emergency. Int J Womens Heal. 2013;5:515
- De Los Rios JF, Castaneda JD, Miryam A. Bilateral ectopic pregnancy. J Minim Invasive Gynecol 2007;14:419–27
- Ghomian N, Lotfalizadeh M. Spontaneous Unruptured Bilateral Tubal Pregnancy: A Case Report. Iran J Med Sci. 2015;40(6):537-540
- Njoku C, Oriji PC, Aigere EOS, Omile C. Spontaneous bilateral ectopic pregnancy: A case report. Yen Med J. 2019;1(1):56-60.
- Andrews J, Farrell S. Spontaneous bilateral tubal pregnancies: a case report. J Obstet Gynaecol Can. 2008;30:51-4.
- Elson C.J, Salim R, Potdar N, Chetty M, Ross J.A, Kirk E.J on behalf of the Royal College of Obstetricians and Gynaecologists. Diagnosis and Management of Ectopic Pregnancy.BJOG 2016; 123: e 15-e55.
- Martinez et.al Martinez J, Cabistany AC, Gonzalez M,Gil O, Farrer M, Romero JA. Bilateral simultaneous ectopic pregnancy. South Med J. 2009;102:1055-7.
- Kwawukume E. Y, Idrisa A, Ekele B.A. Ectopic pregnancy. In: Kwawukume E. Y, Emuveyan E.E (eds). Comprehensive Obstetrics in the Tropics. 2013: 282-287.
- Ikechebelu JI, et al. Laparoscopic Salpingectomy for Ruptured Tubal Ectopic Pregnancy: A Case Report. Ann Med Health Sci Res. 2017; 7:203-205
- Ghomian N Md, Lotfalizadeh M Md. Spontaneous Unruptured Bilateral Tubal Pregnancy: A Case Report. Iranian Journal of Medical Sciences. 2015 Nov;40(6):537-540
- Walter JE, Buckett WM. Spontaneous bilateral chronic and acute tubal ectopic pregnancies following methotrexate treatment. Aust N Z J Obstet Gynaecol. 2004;44:267.