Scoping Review: Pre-Operative Serum Value of Cancer Antigen-125 (CA-125) Assessment as Independent Predictor of Outcome in Endometrial Carcinoma
Shittu, Muhammad Adamu1, Olaoye, Stephen Oyewole1, Umar, Farouk Kabir2
1Department of Obstetrics and Gynaecology, Federal Medical Centre Gusau, Zamfara State, Nigeria
2Department of Radiology, Usman Danfodiyo University Teaching Hospital, Sokoto, Sokoto State, Nigeria
ABSTRACT
There is an upsurge in endometrial cancer (EC) prevalence globally with rising incidence of obesity and more women attaining the postmenopausal milestone. The most important predictor of EC outcome is lymph node metastasis (LNM), and preoperative CA-125 has significant correlation with LNM, advanced disease and survival. This scoping review is aimed at investigating primary studies on role of preoperative CA-125 assessment in predicting outcome of EC and identify gaps for consideration in further studies. Three themes: Populations investigated, optimum cut-off value of preoperative CA-125, and coexisting patients’ demographic, tumor, and radiological parameters in primary studies. The method searched two databases, PubMed and CINHAL to identify primary studies, extract, collate and summarize data and results tabulated, which yielded 199 publications. Fifty met selection criteria and 26 articles met the inclusion criteria. Twenty-six full articles from 13 countries were included; 13 studies were from Europe. Twenty-three articles were retrospective while 3 prospective studies. Only one prospective study was multicenter. One study included only Asian patients while two others did not consider racial preference. Two studies had significant proportion of premenopausal women, 35.7% and 21.4% respectively. Of the 8550-total population across studies, 31.2% were from China. The mean age of patients ranges between 38 and 69 years. Obesity was assessed in eight studies. The cut-off values of CA-125 was 10.9-110.5U/ml and demonstrated diverse correlation with disease outcome with sensitivities and specificities ranges of 27.5-98.6% and 33.0-93.7% respectively; and negative predictive values. Forty-six percent of studies used radiological investigations to support patient evaluation with conflicting findings. In conclusion, high value of preoperative CA-125 predicts LNM, myometrial invasion, disease metastasis and reduced chance of survival in patients with EC and optimum cut-off value are discrepant across studies. Addition of clinical, tumor and radiological parameters to CA-125 values offer conflicting supporting evidence in predicting outcome variable.
Keywords: serum cancer antigen-125, endometrial cancer, survival, lymph node metastasis, lymphatic involvement, metastasis, recurrence.
Correspondence
Dr. Shittu, Adamu Muhammad (FWACS, FMAS, MSc)
Consultant Obstetrician and Gynaecologist
Federal Medical Centre Gusau, Zamfara State, Nigeria
+2348039492682
INTRODUCTION
Endometrial cancer ranks first among female genital tract malignancies 1,2 and its mortality globally is estimated at 76,100 annually.3 Its epidemiology is linked to age and changing lifestyle with more cases in industrialized nations.
Obesity is a major risk factor and with advancing age and associated co-morbidities, treatment outcome might be worse in older patients because of vulnerability to toxicity of treatment. 4 Early stage is curable with overall 5-year survival rate nearly 90%. 5
Age of patient, tumor type grade, TVS, MRI findings, endometrial biopsy and metastasis are indices that predict patients at high risk of poor outcome.2 Sadly, these modalities lack the potential to predict metastatic disease with certainty. 6
Lymph node metastasis is the most important factor in predicting outcome in EC 7, but its involvement is below 15%. 8 Serum cancer antigen 125 (CA-125) value is raised in both primary and recurrent diseases. 9 Majority of investigations on preoperative CA-125 levels in women with EC were conducted in developed countries, 10 with diverse cut-off values. 11
Goksedef et. al. 8 in 2011 reported that elevated level of CA-125 predicts LNM and extrauterine spread of EC with sensitivity of 75% at a cut-off value of 35U/ml. Comparably, a lower cut-off level of 20U/ml demonstrated a correlation between raised CA-125 with LNM and distant metastasis and CA-125 independently predicted LNM and extrauterine spread at the same sensitivity of 75%. 12 Furthermore, Abbink et al. in 2018 suggested raised preoperative serum CA-125 value (cut-off 15U/ml) correlates with myometrial involvement, lymph vascular space invasion (LVSI), and poor disease-free and overall survival. 13 (Conversely, Kotowicz et al. indicated raised serum level of CA-125 (26.3U/ml) is a poor predictor of disease-free and overall survival (DFS and OS). 14
A wide range of studies have utilized different cut-off values of CA-125 achieving results in assessing outcome of EC. Cancer antigen-125 is cheap, reproducible and has the potential to be used in low- and middle-income countries where MRI, CT and PET scan and trained personnel are not readily available. 5
The objective of the scoping review is to identify gaps in primary studies on the role of preoperative serum assessment of CA-125 value in women with endometrial carcinoma.
METHODOLOGY
Research Question
What is the role of preoperative assessment of serum CA-125 value in predicting outcome in women with endometrial cancer?
We identified some knowledge gaps in this question in the published literature from 2011 to 2021.
Search Strategy
After conducting a preliminary search using terms from the research question, relevant key words were identified. PubMed and CINHAL databases were first searched on March 14, 2021, for eligible articles for the scoping review. Using various combinations of key medical search headings (MeSH) and key words, incorporated Boolean operators (AND/OR), truncation (““), and field tags [tw], searches were run on two databases, PubMed and CINHAL. Several key words and terms were used; “endometrial cancer”, “uterine cancer”, “corpus uteri cancer”, “cancer endometrium”, “endometrial carcinoma”, “endometrial neoplasm”, “cancer antigen-125”, CA-125, “preoperative cancer antigen-125”, “preoperative CA-125”, mucin 6, outcome, survival, prognosis, mortality, metastasis, and recurrence.
Inclusion Criteria
Studies included were primary research on preoperative assessment of CA-125 level and related directly to any of the outcome measures, survival, lymph node metastasis or lymphatic involvement, metastasis, and recurrence either independently or in combination. Research articles, full texts, and abstract copies available, limited to human female adults published from 2011 to 2021 and in English language were included in the review irrespective of the study type and country because of increasing interest in the topic in the last decade.
Exclusion Criteria
Excluded from the review were publications of uterine sarcoma, leiomyosarcoma, carcinosarcoma, animal studies, thesis, reports, reviews, personal view, case reports, and letter for authors. All studies on assessment of CA-125 for postoperative monitoring or other tumor markers as predictors of outcome were also excluded.
Review Process
Full texts and abstracts of the articles were screened based on the inclusion and exclusion criteria and studies with no relevance to the research question removed by a single reviewer. The selected articles were compared, duplicates removed using Endnote, and discrepancies resolved. Non-free articles were accessed via the University of Chester institutional access portal and full texts obtained. The reference lists of selected articles were searched and one additional publication that fulfilled the inclusion criteria was included in the review.
Data extraction
After reading the full primary articles included in the scoping review, the following information was extracted, collated, and tabulated on Microsoft Excel spreadsheet and duplicates were stores: authors, country of study, study design, year of publication, number of patients and cut-off value of CA-125. Additional information obtained includes other demographic (age, BMI), tumor and radiologic parameters, factors of interest, sensitivity, specificity, conclusion, and limitation(s) of study. Factors of interest are survival which refers to overall survival (OS), disease-specific survival (DSS), DDS and case-specific survival and disease-free survival (DFS), LNM, recurrence, death, LVSI, and myometrial invasion (MI)and all forms of metastases. Outcomes of scoping review and how they will be presented.
The data was collated using Microsoft Excel spreadsheet and tabulated in duplicates. The outcome of the scoping review are the three themes (1) Populations investigated in primary studies, (2) optimum cut-off value of preoperative CA-125 and (3) coexisting patients clinical, tumor and radiological parameters across primary studies will be presented in tables, graphs, and charts.
RESULTS
The search of the two databases yielded 199 publications, 22 duplicates were removed using Endnote X9 software. The remaining 178 articles were screened by reading their titles and abstracts, 128 articles did not meet the selection criteria. Full copies of the 50 publications that met the selection criteria were read and only 26 articles met the inclusion criteria for this scoping review as shown PRISMA flow chart (Moher, Liberati, Tetzlaff, & Altman, 2010) below.
Scoping Review Outcomes
Population studied in primary articles.
Twenty-six full articles from 13 countries were included in the review with the highest number in 2016 and 2017 (Figure 1). Twelve articles were undertaken in Europe including 8 in Turkey and one each in England, German,
Greece, and the Netherlands. All cases were adult females in their postmenopausal years except in two studies 10,11 that had significant proportion of premenopausal women (35.7% and 21.4%) respectively. The mean age of patients across studies showed wide variation, from 38 years 15 to 69 years 5 and while their age ranges between 21-40 years 10 and 31 -91years. 18 The largest study included on the role of preoperative CA-125 in predicting outcome of EC was conducted in China with 995 patients. 10 Of the aggregate totals of 8550 patients in the primary studies (Table 1), China had 31.2%, whereas Europe had 27.9% with England 5 having only 1.1%. Obesity was assessed in six studies (Table 1.) and predicted to greatly impact on the prevalence of low-grade EC. Three of the 26 primary studies were prospective 5,16,17 and only one was multicenter prospective cohort study. 16 Kang et al; 18 included only Asian patients in a study that had 360 patients from two health institutions. In contrast, two other studies had a robust inclusion criterion with no racial preference from Brazil and Turkey, respectively. 19,20
Optimum cut-off value of CA-125
The optimum cut-off value of CA-125 is unpredictable with varying degrees of sensitivity and specificity across studies as shown in Figure 2. The studies used similar laboratory techniques used to derive the serum level of CA-125 and the serum level is measured in Unit/milliliter (U/ml). Povolotskaya et. al. 5 suggested preoperative cut-off value of CA-125 of 28U/ml correlated with disease outcome parameters, age, and long-term survival with a sensitivity and specificity of 75% and 76% respectively and a high NPV of 95% at excluding LNM for outcome and survival. In contrast, Lin et. al. 20 and Kang et al. 15 using a cut-off value of 35U/ml predicted LNM, MI and extra-uterine malignancy. However, the sensitivity and specificity of this model were 85.9% and 55.5% respectively and a NPV of 97.1%. In the only multicenter prospective cohort study, a lower cut-off value of 17.0U/ml was predictive of disease-free survival of 80.6% and disease-specific survival of 87.1%, relative to 92.1% and
97.2% respectively in low-grade endometrial carcinoma subjects with normal preoperative CA-125 levels. 16
An age-based evaluation of 923 patients using a cut-off value of >35U/ml for patients over 49 years and 105U/ml for those below 49 years predicted LNM, survival and other poor outcomes except tumor grade (table 1). Furthermore, Ünsal et al. determined a cut-off value of >35U/ml of patients < 50 years but contrastingly determined 16U/ml for those over 50 years with a sensitivity and specificity of 71.0% and 60.0% respectively, and a NPV of 87.0 % for the poor prognostic variables. 21 A preoperative cut-off level of 35U/ml predicted LNM with a sensitivity and specificity of 97-99% and 58-64%, thus precluding patients from lymphadenectomy. 4 In disagreement, a study by Sadowski et al. considered patients for lymphadenectomy at a lower cut-off level of 18.5% with a sensitivity and specificity of 94.0% and 91.0% correspondingly and a NPV of 97%. 22
|
Nakamura et al. indicated ovarian metastasis at 56.6U/ml value of CA-125 23 ; this finding differs from that of Lin et. al. that predicted ovarian metastasis at a cut-off value of 110.5U/ml with a sensitivity and specificity of 74% and 93% respectively.20
An optimum value of CA-125 of 10.9U/ml independently predicted disease-free survival.14 Contrastingly, Reijnen et. al. suggested a cut-off value of 66.0U/ml independently predicted DFS and DSS for all grades of endometrial carcinoma. 16
Demographic characteristics, tumor, and radiological parameters
The 26 primary studies reported on these parameters (Table 1) and illustrated in Figure 3. These are tumor, demographic (age, MI), and radiological parameters included in preoperative risk assessment and could be of prognostic significance. Low-grade tumor with elevated CA-125 is considered a high-risk factor for myometrial invasion, advanced disease, and mortality. 16 Unfavorable tumor grade and histology also strongly predicted patient survival (Chi square=36.5, df=4, p=0.001) ahead of elevated CA-125. But among patients with endometroid-type carcinoma, elevated CA-125 is a strong predictor of survival (Chi square=6.039, df=2, p=0.02) whereas grade of the tumor poorly predicted survival. 5
Jiang et. al. 10 reported that histologic grade 3 EC is an independent predictor of outcome variables with a corresponding sensitivity and specificity of 60.2% and 60.0%. 10,19 indicated tumor grade (p<0.001) and tumor size (p<0.001) were good predictors of LNM with AUC of 0.858.
Kang et al. suggested MRI predicts MI, CI, extrauterine spread and LNM (p=0.04, p<0.001 and p<0.001 respectively) with sensitivity and specificity of the model as 84.9% and 55.5% and a NPV of 91.7% (Table 1). 17 Deep myometrial invasion ≥50% on preoperative MRI was accurate in 78.3% of the 310 patients studied and distinguished deep from superficial invasion with a sensitivity and specificity of 85.1% and 71.8% correspondingly. 24 Abdominal CT-scan in patients with low-grade tumor did not show correlation with disease outcome variables (Table 1). Sadowski et. al. identified patients for lymphadenectomy and reported an improvement in LNM detection from about 4.0% to 11.1% in presence of positive preoperative MRI findings, but no impact on detection of MI and metastasis in low-grade EC. 22 Contrastingly, a correlation was found between ADCmin on MRI with stage (p=0.001), LNM (p=0.027), and metastasis (p<0.05). 23 A combination of MRI and CT predicted MI, LVSI and LNM with odd ratios of 2.12, 2.98 and 6.49 correspondingly; and used a cut-off value of 21.5u/ml to investigate the combination of variables best at predicting LNM. 18 Furthermore, Zhuo et. al. predicted
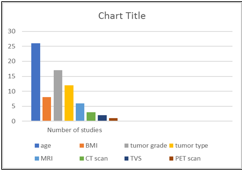
Figure 3. Frequency of coexisting parameters assessed per study.
LVSI and at comparably similar CA-125 value of 21.2U/ml. 25 In a statistical model, ADCmin on MRI of the primary malignancy could independently predict EC recurrence. Another study revealed that SUXmax on PET/CT of primary tumor better predicted poor prognosis in patients with EC (P=0.025). 23 Lee et. al. predicted LNM by use of Transvaginal ultrasound scan (TVS) with a sensitivity of 94% and specificity of 57%. 26
DISCUSSION
The prevalence of studies on the role of preoperative CA-125 value as a predictor of outcome in patients with EC has increased remarkably from 2016 to 2017 accounting for 46.1% of the total, and 46.1% of the studies were conducted in Europe (table 1). 26,27 This increase in prevalence is like reported by Patsner et al. 9 The recent studies have given attention to other preoperative clinico-pathologic and radiologic parameters combined with preoperative CA-125 assessment to improve the validity of the models in predicting outcomes of EC. There were more retrospective studies 10,20 using hospital records to ascertain the role of preoperative CA-125 in predicting outcome of EC. Among the 26 studies, only three were prospective 5,15,16 and recruited patients consecutively: however, Reijnen et. al. in a multicenter cohort study used the same recruitment approach. 16 This suggests a gain in experience in evaluating the role of preoperative assessment of CA-125 value in predicting outcome of EC.
Lifestyle and sociodemographic factors were risk factors of EC and were inconsistently reported across studies, making it difficult to exclude influence of diseases on outcomes. 10,19 Interestingly, being overweight or obese confers the advantage of a minimal risk of LNM and increased incidence of low-grade endometroid type cancer. 36 Contrastingly, it was indicated that lower body mass index poses a greater risk of LNM in EC. 37 These discordant views could make the decision on routine lymphadenectomy difficult to make with its attendant debilitating complication. This could further be compounded by the effect of advanced age. 3
Several studies cited discrepant cut-off values of preoperative CA-125 in assessing women with EC with varying degree of sensitivities and specificities at predicting its outcome. Eleven studies set a cut-off value around 35U/ml 8,29,30 while about half of these set lower values with correspondingly lower sensitivities and specificities 5,14,16 Studies with cut of values above 35U/ml, for instance 110.5U/ml did not show remarkable difference in sensitivity and specificity in predicting outcome variables. 20
Nakamura et. al. and Ling et al. suggested that a higher cut-off value of CA-125 could independently predict higher DFS and OS. 20,23,31This was corroborated by Reijnen et al. 16 In contrast, Kang S. et. al. and Biler et. al. indicated that a lower value of 10.0U/ml was an independent predictor of both DFS and OS. 14,15 Furthermore, a lower cut-off value even in low-grade EC independently predicted disease survival irrespective of other poor prognostic parameters, thus emphasizing the significance of preoperative CA-125 level in predicting patient survival. 14
These inconsistencies might have resulted from differences in the study designs (and the variation in reagents and techniques utilized in the assay of preoperative Ca 125). The majority were retrospective, single institutional and some with selection biases as limitation.
Lymph node involvement as the most important predictor of outcome in EC ⁶ occurs in approximately 15% following surgery. 7,9 Its identification has been made easy with a combination of preoperative MRI and CA-125 with good sensitivity. 15 With expensive preoperative MRI, detection has not remarkably improved. 23 MRI detected rather fewer (11.1%) LNM as indicated recently. ²² With these findings, it remains uncertain whether patients with elevated preoperative CA-125 could be subjected to routine MRI solely to detect LNM. Similarly, TVS deployed to predict patients at high risk of poor outcome lacks the potential to predict metastasis with certainty. 5 A more recent study indicated that TVS used in combination with preoperative CA-125 assessment predicted LNM at a CA-125 cut-off value of ≥35U/ml with a sensitivity and specificity of 94.0% and 57.0% respectively. 26 This could be of much utility especially in low-resource settings where high-end technological investigation modalities and trained personnel are not readily available.
The limitations of this scoping review are restricted to two databases, published articles in English language and conducted by a single reviewer.
CONCLUSION:
High value of preoperative CA-125 is a risk for lymph node metastasis, myometrial invasion, disease metastasis and reduced chance of survival in patients with endometrial carcinoma though the optimum cut-off value is diverse across studies. Addition of coexisting parameters to CA-125 values offer conflicting supporting evidence in predicting outcome variables. It would probably require more rigorous worldwide clinical trials to address these gaps in previous studies.
REFERENCES