

![]()
Sonographic Placental Morphology and the Risk of Preeclampsia and Delivery of Small for Gestational Age Baby at a Nigerian South-West Tertiary Hospital
Obilade Adekunle O 1, Akinmoladun Janet A 2, Olanlege Shakirat O1, Arowojolu Ayodele O3
1Department of Obstetrics and Gynaecology, Adeoyo Maternity Teaching Hospital, Ibadan, 2Department of Radiology, College of Medicine, University of Ibadan /University College Hospital, Ibadan; 3Department of Obstetrics and Gynaecology, College of Medicine, University of Ibadan/University College Hospital, Ibadan.
ABSTRACT
Introduction: Pre-eclampsia (PE) is a disease of public health importance because of its associated maternal and perinatal morbidity and mortality. This study aimed to determine the association between early 2nd trimester placental morphology and subsequent risk of developing PE and/or delivery of small for gestational age (SGA) neonate. Method: This was a prospective cohort study conducted at the Adeoyo Maternity Teaching Hospital, Ibadan, over a one-year period. Pregnant women who met the criteria were recruited for the study from gestational age of 15weeks + 0day to 19weeks + 6days. Maximum placental thickness and length were measured during routine obstetric ultrasound and the participants were followed up till delivery. Association between placental thickness and PE and/or SGA was tested. The mean placental length between pre-eclamptic and normotensive groups were compared using independent sample t-test. Data analysis was done using IBM SPSS, version 26. Ethical approval for the study was obtained. Results: One hundred and eighty-six women were recruited for the study. Placental thickness above normal in the early 2nd trimester was significantly associated with PE (P<0.001). However, the association was not statistically significant after adjusting for confounders–maternal risk factors (AOR=0.5, 95% CI: 0.05 to 6.0, P=0.6). Placental thickness below normal was significantly associated with SGA (P=0.04), but no significant association was found between early 2nd trimester placental length and preeclampsia (P=0.5) and SGA (P=0.64). Conclusion: There was an association between placental thickness in the second trimester and the risk of developing preeclampsia/ small for gestational age. However, no significant association was found with placental length
Keywords: Sonography, Preeclampsia, Small for Gestational Age, Placental Thickness, Placental length
Corresponding author:
Dr Janet A Akinmoladun
Department of Radiology, College of Medicine,
University of Ibadan /University College Hospital, Ibadan
08024747372
INTRODUCTION
Preeclampsia is a disease of public health importance because of its associated maternal and perinatal morbidity and mortality.1,2Globally, it complicates 2-10% of all pregnancies [2] while the incidence varies from 1.2-8.8% within Nigeria.3-5 Preeclampsia ranks as the second leading cause of maternal mortality worldwide accounting for 10-15% of maternal death, only preceded by haemorrhage.6,7
According to the International Society for the Study of Hypertension in Pregnancy (ISSHP), Preeclampsia is defined as Gestational Hypertension accompanied by one or more of the following new-onset conditions at or after 20 weeks of gestation: (1) Proteinuria (2) Maternal organ dysfunction e.g., acute kidney injury, Liver complications, Neurological complications, Hematological complications etc. and (3) Uteroplacental dysfunction.8
Preeclampsia (PE) has been shown to be closely associated with Small for Gestational Age (SGA). There is an inverse relationship between gestational age at delivery and the prevalence of SGA. The prevalence of SGA in pregnancy complicated by PE who delivered at less than 34 weeks, between 34 and 37 weeks and greater or equal to 37 weeks are 82%, 47% and 30% respectively, whereas the prevalence of SGA in pregnancies without PE who deliver at these gestational ages are 44%, 21% and 8% respectively.9
The most widely used method of screening for preeclampsia is identification of risk factors from maternal demography and medical history.10-12 Although identification of maternal risk factors is useful, it is not an efficient screening tool for preeclampsia.13 Most of the other screening methods available today use biophysical method for assessing the placental changes or biochemical method identifying the biomolecules that are produced in response to hypoxia caused by reduced placental perfusion in preeclampsia. Many of them are still not widely acceptable because of low detection rate and high false positivity.14
If the disease could be accurately predicted, preventive measures, such as the use of low dose aspirin (LDA) and calcium intake (in area where there is low dietary calcium intake), could be instituted.8,14 Other measure includes increased surveillance for early diagnosis and institution of appropriate treatments to reduce morbidity and mortality associated with the disease.[8]
The pathogenesis of preeclampsia has been closely linked to abnormalities in placental development2,15-17 and the placenta has been implicated as the root cause of preeclampsia. Preeclampsia begins to abate with the delivery of the placenta and can occur in the absence of a fetus but with the presence of trophoblast tissue as seen in molar pregnancies.18
The morphology of the placenta in terms of weight, surface area, volume, shape and thickness has been shown to be affected in preeclampsia.18-20 Ultrasonography is a non-invasive modality for screening for preeclampsia and the use of two-dimensional ultrasound has been shown to be simple, rapid and an accurate tool in estimating placenta dimensions.21,22 Also, a study by Miwa et al23 shows that ultrasonographic measurement of placental thickness is a simple way of measuring placental size and that thick placenta is a predictor of adverse pregnancy outcome. The study of placental morphology early in pregnancy by a simple noninvasive tool such as 2-Dimensional ultrasonography may be able to give predictive features for preeclampsia later in pregnancy. This is particularly important for a low resource country like Nigeria. Ultrasound measurement of placental thickness and length is a simple, relatively inexpensive tools that can be employed at all levels of health care delivery (primary, secondary and tertiary) for screening patients for preeclampsia.
There is also paucity of data regarding the association of placental thickness and length, with occurrence of preeclampsia in the literature. This study aimed to determine the association between early 2nd trimester placental morphology and subsequent risk of developing preeclampsia and/or delivery of small for gestational age (SGA) babies.
MATERIALS AND METHODS
This was a prospective cohort study involving pregnant women attending the antenatal clinic in Adeoyo Maternity Teaching Hospital Ibadan (AMTH). These participants were selected using purposive sampling method and the study spanned a period of 12 months. All consenting pregnant women with viable singleton fetus who presented at the booking clinic with gestational ages between 15 weeks +0 day to 19weeks + 6day were recruited. The exclusion criteria were: multiple gestation, chronic hypertension, chronic renal disease, pre-existing diabetes mellitus, gestational diabetes mellitus, congenital anomaly of the uterus, congenital anomaly of the fetus, sub-chorionic haematoma, maternal anaemia, sensitized rhesus negative mothers, polyhydramnios, low-lying placenta, grossly eccentric cord insertion. The participants were followed up for an average of 20 weeks. The day of discharge after delivery was taken as the end point for each participant.
The following information were documented; biodata, the date of the first day of last menstrual period (LMP), obstetrics history and past medical history. The height, weight, booking body mass index (BMI) and blood pressure of each selected participant were also recorded.
The gestational age (GA) was estimated from the patient’s first day of the last menstrual period (LMP). When a participant was not sure of her LMP or there was a disparity of more than 10 days from the GA given by an early ultrasonography (US) done on or before recruitment at 19 weeks GA, early US date was used.24
Two-dimensional ultrasound Scanning was done in the antenatal clinic using Versana Essential ultrasound machine (made by General Electric Co., China) equipped with a 3-5 MHz multifrequency curvilinear transducer. Fetal biometry taken included biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC) and femur length (FL). Maximum Placental Thickness (in millimeters) was measured at the middle of the placenta just beside the umbilical cord insertion. The measurement was taken from chorionic plate to the sub-placental veins while ensuring that the calipers were perpendicular to the uterine wall which was excluded in the reading. Maximum Placental Length was measured along the longest diameter of the placenta after scanning in two perpendicular planes. Three measurements each of the placental thickness and length were taken, and the average was used as the observed value.
After delivery, participants’ records were retrieved and information on diagnosis of preeclampsia, GA at delivery and birthweight were extracted. Preeclampsia was diagnosed by using ISSHP criteria8 while small for gestational age (SGA) was diagnosed when the birthweight was below the 10th percentile for the age in a standard birthweight curve [25] used in a Nigerian population.
Ultrasound measured maximum Placental Thickness (PT) was divided into three categories viz: normal, above normal, and below normal for gestational age using the nomogram for Nigerian population derived by Adeyekun et al.26 The occurrence of PE and SGA were compared among the three categories. Association between placental thickness and preeclampsia, and placental thickness and SGA were found using chi-square for trend. Logistic regression analysis was used to determine significance of the association between preeclampsia, SGA, and other variables related to the participants in this study.
The mean placental length of participants who developed preeclampsia was compared with the mean placental length of the participants who did not have preeclampsia using independent sample t-test. P-value <0.05 was taken as the level of statistical significance.
Data analysis was done using IBM statistical package for social sciences (SPSS), version 26. The results were presented in the forms of tables and charts.
Ethical clearance was obtained from Oyo State Research Ethical Review Committee, Ministry of Health, Government Secretariat, Ibadan. Written informed consent was also obtained from each participant.
RESULTS
One hundred and eighty-seven women participated in the study. One hundred and fifty-one (80%) participants were followed up till delivery while the others (36, 20%) were lost to follow-up. The modal age group was 26-30, consisting of 56 (37.1%) participants while only 1(0.7%) participant was in age group less than 20. Majority of the women were primigravida (62, 41%) while 14(9.3%) were with their 5th or more pregnancy. Sixteen (10.6%) of these 151 participants developed preeclampsia while 14(9.3%) were diagnosed with gestational hypertension. No significant association between preeclampsia and maternal age (P=0.861) and preeclampsia and number of pregnancy (number of gravidity) (P=0.788) (Table 1)
Table 1: Maternal Blood Pressure Outcome Versus Maternal Age and Number of Pregnancies (Gravidity).

One hundred and two (67.5%) of the 151 participants had normal placental thickness, 45(29.8%) had above normal placental thickness (thicker placenta) while 4(2.7%) had below normal placental thickness (thinner placenta). Four (2.7%) of the participants delivered SGA babies and only one of these had preeclampsia (Table 2)
There was a significant association between early 2nd trimester placental thickness and preeclampsia (P<0.001) with participants with thicker placental more likely to develop preeclampsia compared to participant with normal or below normal
Table 2: Association Between Placental Thickness, Preeclampsia and SGA.

Table 3: Relative Risks of Preeclampsia and SGA when there is Abnormal Placental Thickness (PT).

*Abnormal Placental Thickness: Above Normal (Thicker) Placental Thickness + Below Normal (Thinner) Placental Thickness.
placental thickness. There was also a significant association between early 2nd trimester placental thickness and SGA (P<0.001) with participants with below normal (thinner) placental thickness more likely to deliver SGA babies. However, the association between placental thickness and preeclampsia with SGA was not statistically significant (P=0.31), (Table 2).
Table 4: Independent Sample t-test Comparing Mean Placental Length in the Normotensive Group and Mean Placental Length in the Pre-eclamptic Group.

Table 5(a): Logistic Regression Analysis of Association between Potential Factors and Preeclampsia, SGA and Gestational Hypertension.

COR: crude odd ratio; *Significant P-value
Table 5(b): Multiple Logistic Regression Analysis of Association between Potential Factors and Preeclampsia, SGA and Gestational Hypertension

AOR: adjusted odd ratio; *Significant P-value
There was a significant risk of developing preeclampsia when early 2nd trimester placental thickness was above normal (RR=10.0, 95% CI: 2.7 to 30.0, P=0.01), It was also found that there was a significant risk of delivery SGA babies when there was abnormal (thinner or thicker) placental thickness (RR= 6.3, 95% CI: 0.7 to 58.5, P<0.001) with the risk becoming extremely larger when there was a thinner placenta (RR= 50.0, 95% CI: 0.7 to 58.5, P<0.001), (Table 3).
There was an 8-point difference in the mean placental length between the patients that developed PE and the normotensive women, however, this difference was not statistically significant (P=0.5), (Table 4). This means that early 2nd trimester placental length was not significantly associated with preeclampsia.
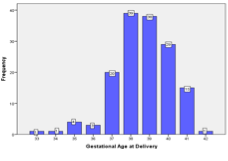
Figure 1(a): Gestational Age at Delivery Among all the Participants.

Figure 1(b): Gestational age at Delivery among the Preeclamptic Participants.
Table 5(b): Multiple Logistic Regression Analysis of Association between Potential Factors and Preeclampsia, SGA and Gestational Hypertension

Figures 1 (a) and 1 (b) show gestational age of delivery among the participants. Gestational age at delivery ranges from 33 to 42 weeks with most participant delivered between 37 and 41 weeks. The gestational age at delivery among the preeclamptic participants was also spread within this range with modal gestational age at delivery of 37 and 38 weeks (6 out of 16, 37.6%). One participant (6.3%) each delivered at 33, 34, 36 and 40 weeks. Two participants (12.5%) each delivered at 35, 39 and 41 weeks. This implies that only one participant (6.3%) had Early-Onset Preeclampsia, all other (15, 93.7%) had Late-Onset Preeclampsia. It is also worthy of note that 3(18.9%) of the Late-Onset Preeclampsia were Preterm Preeclampsia, others (12, 74.8%) were Term Preeclampsia.
A logistic Regression Analysis shows that the booking BMI was the most important other risk factor for PE, SGA and gestational hypertension in this study (COR=3.1, 95% CI: 1.1 to 9.1, P=0.038 Table 5(a)). However, the risk for SGA when there was below normal placental thickness persists after adjusting for maternal age, number of pregnancies and the booking BMI (AOR= 40.6, 95% CI:2.0 to 81.9, P=0.02, Table 5(b)).
There was a risk of developing gestational hypertension when there was a thicker placenta. However, the risk was not statistically significant (COR=2.3 95% CI: 0.75 to 6.9, P= 0.15, Table 5(a)). After adjusting for maternal age, number of pregnancies and booking BMI, the risk normalizes (AOR=0.508, 95% CI: 0.158 to 1.630, P=0.26, Table 5(b)).
Logistic regression analysis showed that there was no significant association between early 2nd trimester placental length and SGA (COR=0.995, 95% CI: 0.977-1.015, P=0.64, Table 5(a)). There was also no association between placental length and gestational hypertension (COR= 1.0, 95% CI: 0.99 to 1.02, P=0.16, Table 5(a)).
DISCUSSION
The incidence of preeclampsia in this study was 10.6% which is slightly higher than 1.2-8.8% found in the previous studies within Nigeria3-5 but within the global incidence of 2 -10%.2 The higher incidence in this study may be attributed to the strict diagnosis of preeclampsia using ISSHP guideline which was not used in the other studies.
The finding of a significant association between early 2nd trimester placental thickness and preeclampsia in this study is similar to the finding in a prospective cohort study of first trimester placental thickness and the risk of preeclampsia or SGA by Vachon-Marceau et al.27 However, the relationship became non-statistically significant after adjusting for the confounders (maternal age, booking BMI and number of pregnancies) in this study. The possible reason for the non-statistically significant relationship may be due to the smaller sample size in this study compared to Vachon-Marceau27 study. The finding is however, at variance with the findings of Tiruneh [20] and Goswami [28] who found that thinner placentae were associated with preeclampsia and pregnancy induced hypertension (PIH) respectively. This variation could be due to their method of data collection, as the average of three measurements of the maximum placental thickness was taken as the observed value in this study compared to an average of multiple measurements from center to the periphery of the placenta used in these those two studies. Also, Goswami did not differentiate preeclampsia from gestational hypertension, the two groups were assessed together as PIH.
The study also found that there was a significant association between early 2nd trimester placental thickness and SGA with the participants with thinner placental having a significant risk of delivering babies with SGA. The risk remained significant after adjusting for maternal age, BMI and number of pregnancies. This finding is similar to the finding of previous studies by Vachon-Marceau et al27 and Adeyekun26 and slightly varies from other previous studies20,29,30 who found reduced placental thickness and birthweight in participants with preeclampsia. This variation may be due to study design as they were looking at placental morphology and birth weight in the normotensives and preeclamptic cohorts while this research studied association between placental morphology and birthweight.
There was no significant association between early 2nd trimester placenta length and preeclampsia. This is divergent from previous studies20,28-30 who found that the placenta length or widest diameter was smaller in the preeclamptic group compared to normotensives. This may be due to differences in the timing of data collection. In this study, the placental morphological measurements were taken in the early 2nd trimester, at which time the placenta is still undergoing proliferation and remodeling.31 Those studies that found reduced placenta length in the preeclamptic patients took a gross morphometric measurement of the placenta after delivery. It has been shown that placental length and surface area tend to reduce as pregnancies advance in preeclampsia due to ischaemia and infarction caused by placenta hypoxia.18
The increase in placenta thickness in the early part of the second trimester in patients that would later develop preeclampsia is thought to be compensatory for restricted expansion of the surface area, so as to enhance oxygenation. Hypoxia resulting from impaired trophoblastic invasion of the spiral arterioles is worse in the periphery of the placenta, resulting in ischaemia and infarction at the periphery and reduction in the surface area and diameter (width or length). In an attempt to compensate for the hypoxia, there is increase in trophoblastic proliferation and branching of villi which is more at the center that is richer in blood supply, resulting in increased placental thickness at the center.18,32
There was a risk of developing gestational hypertension when there was a thicker placental which was not statistically significant. Although, the association between placental thickness and gestational hypertension was not statistically significant, it may be clinically relevant when combined with maternal risk factors such as age, BMI etc. bearing in mind that gestational hypertension may be a precursor for preeclampsia. There was no significant association between placental length and gestational hypertension in this study.
CONCLUSION
There was an association between placental thickness in the second trimester and the risk of developing preeclampsia/ small for gestational age. However, no significant association was found with placental length.
Funding: Nil
Conflict of interest: Nil
REFERENCES
- Osungbade KO, Ige OK. Public health perspectives of preeclampsia in developing countries: Implication for health system strengthening. J Pregnancy.2011; 2011:481095.
- Rosner JY, Mehta-Lee SS. Hypertension in Pregnancy. In: DeCherney A. H, Nathan L. (eds.) Current Diagnosis and Treatment Obstetrics and Gynecology. 12th ed. USA: The McGraw-Hill Company; 2019. p.454-465.
- Kooffreh ME, Ekott M, Ekpoudom DO. The prevalence of pre-eclampsia among pregnant women in the University of Calabar Teaching Hospital, Calabar. Saudi J Health Sci. 2014; 3(3):133-136.
- Singh S, Ahmed EB, Egondu SC, Ikechukwu NE. Hypertensive disorders in pregnancy among pregnant women in a Nigerian Teaching Hospital. NigerMed J. 2014; 55(5):384-388.
- Musa J, Mohammed C, Ocheke A, Kahansim M, Pam V, Daru P. Incidence and risk factors for pre-eclampsia in Jos Nigeria. Afri Health Sci. 2018; 18(3): 584-595.
- Ghulmiyyah L, Sinai B. Maternal mortality from preeclampsia/eclampsia. Seminars in Perinatology. 2012; 36(1):56-59.
- Say L, Chou D, Gemmill A, Tunçalp O, Moller A, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2(6):e333.
- Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018; 13:291–310.
- Yu CK, Khouri O, Onwudiwe N, Spiliopoulos Y, Nicolaides KH. Prediction of pre-eclampsia by uterine artery Doppler imaging: Relationship to gestational age at delivery and small-for-Gestational age. Ultrasound Obstet Gynecol. 2008; 31(3):310–313.
- Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. Screening for preeclampsia: US Preventive Services Task Force Recommendation Statement. JAMA. 2017; 317(16):1661–1667.
- World Health Organization. WHO Recommendations for Prevention and Treatment of pre-Eclampsia and Eclampsia. Geneva: WHO; 2011, Updated 2018. Available from: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/9789241548335/en/ [Accessed 19 March 2020].
- Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 2014; 4(2):97–104.
- Wallenburg HC. Prevention of pre-eclampsia: Status and perspectives 2000. Eur J Obstet Gynecol Reprod Biol. 2001; 94(1):13–22.
- Poon LC, Shennan A, Hyett JA, Kapur A, Hadar E, Divakar H, et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet. 2019; 1(Supp 1):1-33. Erratum in: Int J Gynaecol Obstet. 2019; 146(3):390-391.
- Fisher SJ. Why is placentation abnormal in preeclampsia? AJOG. 2015; 213(4): S115–S122.
- Redman CWG, Staff AC. Preeclampsia, biomarkers, syncytiotrophoblast, stress, and placental capacity. AJOG. 2015; 213(4):S9.e1–S9-11.
- Burton GJ, Yung HW, Cindrova-Davies T, Charnock-Jones DS. Placental endoplasmic reticulum stress and oxidative stress in the pathophysiology of unexplained intrauterine growth restriction and early onset preeclampsia. Placenta. 2009; 30 Suppl A(Suppl):S43–48.
- Roberts JM, Escudero C. The Placenta in preeclampsia. Pregnancy Hypertens. 2012; 2(2):72–83.
- González-González NL, González DE, Padrón E, Armas G M, Plasencia W. Value of Placental Volume and Vascular Flow Indices as Predictors of Early and Late Preeclampsia at First Trimester. Fetal Diagn Ther. 2018; 44(4):256-263.
- Tiruneh ST. Correlation between gross morphology of the human placenta and birth weight in normotensive and pre-eclamptic pregnancies in Northwest Ethiopia. Anatomy. 2018; 12(1):27–32.
- Guiot C, Gaglioti P, Oberto M, Piccoli E, Rosato R, Todros T. Is three-dimensional power doppler ultrasound useful in the assessment of placental perfusion in normal and growth-restricted pregnancies? Ultrasound Obstet Gynecol. 2008; 31(2):171–176.
- Azpurua H, Funai EF, Coraluzzi LM, Doherty LF, Sasson IE, Kliman M, et al. Determination of placental weight using two‑dimensional sonography and volumetric mathematic modeling. Am J Perinatol. 2010; 27(2):151‑155.
- Miwa I, Sase M, Torii M, Sanai H, Nakamura Y, Ueda K. A thick placenta: a predictor of adverse pregnancy outcomes. Springer Plus. 2014; 3:353.
- American College of Obstetricians and Gynecologists. Methods for Estimating the Due Date. Committee Opinion No. 700. Washington DC: ACOG. 2017; 129: e150–154.
- Mokuolu OA, Adesiyan OO, Suleiman MB, Bello M. Intrauterine growth standards: a cross-sectional study in a population of Nigerian newborns. Pediatr Rep. 2012; 4(3): e29.
- Adeyekun AA, Ikubor JE. Relationship between two-dimensional ultrasound measurement of placental thickness and estimated fetal weight. Sahel Med J. 2015; 18(1):4-8
- Vachon-Marceau C, Demers S, Markey S, Okun N, Girard M, Kingdom J, et al. First-trimester placental thickness and the risk of preeclampsia or SGA. Placenta. 2017; 57:123-128.
- Goswami PR, Shah SN. Placenta in normal and pregnancy induced hypertension in relation to its clinical significance: a gross study. Int J Sci Stud. 2016; 4(7): 58-61.
- Maduray K, Moodley J, Naicker T. Morphometrical analysis of placental functional efficiency in normotensive versus preeclamptic South African black women. Pregnancy Hypertens. 2016; 35(3): 361-370.
- Marques MR, Grandi C, Nascente LMP, Cavalli RC, Cardoso VC. Placental morphometry in hypertensive disorders of pregnancy and its relationship with birth weight in a Latin American population. Pregnancy Hypertens. 2018; 13:235–241.
- Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Case BM, et al. Placentation, Embryogenesis and Fetal Development. Williams Obstetrics. 25th ed. USA: McGraw-Hill Education; 2018. p.185-326.
- Kajantie E, Thornburg K, Eriksson JG, Osmond L, Barker DJ. In preeclampsia, the placenta grows slowly along its minor axis. Int J Dev Biol. 2009; 54(2-3):469-473.
- Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental imaging: normal appearance with review of pathologic findings. RadioGraphics. 2017; 37(3):979–998.
- Lee AJ, Bethune M, Hiscock RJ. Placental thickness in the second trimester: a pilot study to determine the normal range. J Ultrasound Med. 2012; 31(2):213–218.
- Thurston M, Weerakkody Y. Placental thickness. Radiopaedia. updated 2018. Available from: https://radiopaedia.org/articles/placental-thickness [Accessed 2nd April 2020].