Conservative Management of Inaccessible Genitourinary Fistula: Case Report and Literature Review
Adebayo Babafemi Charles Daniyan, Sulaiman Bilal, Richard Offiong, Nnenna Egbonwonu,
Chinonso Okere, Arinze Chukwu, Sumayya Adamu, Emmanuel Ochuma
Department of Obstetrics and Gynaecology, University of Abuja Teaching Hospital, Abuja, Nigeria
ABSTRACT
ABC Daniyan
Dept of O&G, UATH, Abuja
abcdaniyan@gmail.com
INTRODUCTION
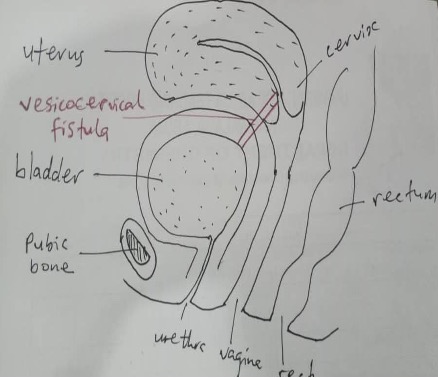
Obstetric fistula is a common cause of urinary incontinence among women in the low- and middle-income countries.1 The continuous leakage of urine significantly reduces the quality of life of affected women.2 It is also associated with profound stigma, shame, guilt, low self-esteem, mental and psychosexual problems.2.3 It is a common morbidity following prolonged obstructed labour and poorly-performed Caesarean section.4,5 Iatrogenic fistulas following Caesarean section done in the late first or the second stage of labour may result in rare types of fistulas such as vesicocervical or vesicouterine fistulas.5,6 These fistulas are usually inaccessible clinically, necessitating endoscopic and radiological procedures to delineate.
Conservative management with the Foley catheter is recommended if obstetric fistula is diagnosed within 4 weeks of delivery (i.e. fresh fistula). The catheter is retained in the bladder for 4 weeks. Its advantages include cost effectiveness, safety, simplicity and availability, making it beneficial in a low-resource setting.7,8 It also shortens the period of medical and social rehabilitation of the women thereby preventing them from becoming outcasts.9 About 25% of women with fresh fistulas will achieve closure and will be continent following conservative management with the Foley catheter.10 A recent study however estimated that 67-100% of women with obstetric fistula can be successfully managed conservatively.11
In many low- and middle-income countries where obstetric fistula is prevalent, facilities like cystoscopy, hysteroscopy, endoscopic sonography and radiological procedures to accurately characterize fistulas are lacking. Hence it may not be feasible to determine the exact site and size of some fistulas due to anatomical location. Evaluation of such patients is largely clinical in these low-resource settings. Therefore, women with such fistulas, if fresh, should benefit from conservative management. This is expected to increase the success rate more than what has been documented. The aim of this case report is to highlight this clinical scenario and to review the literature on the subject.
CASE PRESENTATION
A 32-year-old Para 9+0, 4 alive presented on self-referral at the Urogynaecology Clinic 26 days after an emergency Caesarean section with complaints of urinary incontinence of 21 days duration. Her last pregnancy was unsupervised. She was in labour at home for 24 hours and later taken to a hospital for an emergency Caesarean section. Outcome was a live male neonate. Leakage of urine started after the urinary catheter was removed on the fifth postoperative day. There was no history of voluntary voiding. She was not a known hypertensive or diabetic.
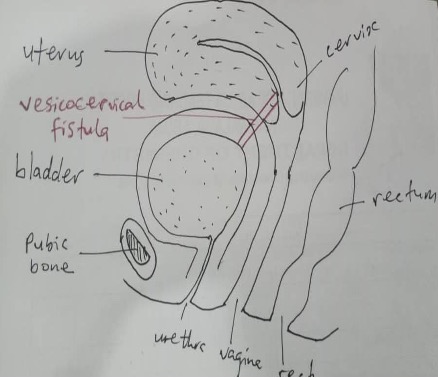
Figure 1 Possible location of an inaccessible genitourinary fistula

Figure 2 Intact Anterior Vaginal Wall In An Inaccessible Genitourinary Fistula
Physical examination revealed a sad-looking young woman. She was not pale and was well nourished. Her cardiovascular and respiratory systems were normal. Abdominal examination showed a transverse suprapubic scar. There was no tenderness, no organomegaly. Vaginal examination revealed intact female external genitalia, wet vulva, patent urethra, good vaginal depth, no anterior or posterior vaginal wall defect. Cervix was not palpable. Urine was seen leaking from the upper end of the vagina, but the cervix was not seen. Methylene blue dye test was positive, but the fistula was not visualised and inaccessible. An impression of genitourinary fistula was made.
She was informed of the findings. She was counselled for conservative management, and she consented. A size 18 Foley catheter was inserted and was inflated with 10mls of sterile water. She was encouraged to drink 3 litres of water daily. She was seen 4 weeks later. Methylene blue dye test was negative, and catheter was removed. There was no leakage of urine. She was seen after another 4 weeks and there was no leakage of urine. She was happy and was discharged from the clinic. She was counselled on sexual abstinence for 3 months and the need for family planning for a minimum of 6 months. She was referred to the Family Planning Clinic. She was also counselled to utilise antenatal care services in her next pregnancy and delivery by elective Caesarean section.
DISCUSSION
The burden of obstetric fistula in Nigeria is enormous, comprising both the women awaiting repair and those developing fresh fistulas.12The need to reduce this burden as well as the priority areas of interest are well articulated in the current national strategic framework for elimination of fistula.7 That policy document identified increased use of bladder catheterization for the management of fresh fistulas as one of the key activities to reduce the prevalence of untreated fistulas. This is recommended as the the first line approach for the treatment of fresh non-ureteric urinary obstetric fistula and for prevention of urinary fistula of obstetric and non-obstetric bladder injuries. Fistulas from malignancies, radiotherapy, and infections should however be excluded.7 Although the use of catheter is not a new practice, there is need to increase the number of women benefitting from catheter care. The case presented highlights the effectiveness of conservative management in an inaccessible fistula.
Conservative management with catheter as the sole treatment strategy was popularized by Kees Waaldijk who found it to be highly effective for fresh fistulas.13 The catheter is inflated with 10ml of sterile water and retained in the bladder for 4 weeks.14 This method of treatment is easy, cheap, safe, available, community-based and facilitates rehabilitation.7,9,14 If successful, it also helps to avert surgical repair as in the case presented.14
Fresh fistulas are the ones diagnosed within four weeks of injury.14,15 The immediate result of prolonged obstructed labour is ischaemic necrosis of the bladder and vaginal/cervical tissues followed by sloughing of devitalized areas.16 The immediate result of iatrogenic bladder injury is inflammation with oedema. Catheterization at this stage achieves bladder decompression by continuous draining of urine, apposing the injured or cut edges, thereby facilitating healing. It also prevents detrusor contractions to empty the bladder and improves blood supply thereby allowing closure of the wound created by sloughing of devitalized tissues either due to ischaemic necrosis or inflammation, before tract formation and epithelization occurs.15 In the case presented, the woman presented 26 days after the injury. Majority of women with obstetric fistula however do not present this early thus missing the opportunity for catheter care. The average duration of symptoms before presentation for obstetric fistula repair in our environment is 42 months.17
Assessment of fistula location and size is a routine procedure as majority of fistulas can be accessed during speculum vaginal examination of fistula patients. Rarely, endoscopic and radiological procedures may be needed to achieve this in some inaccessible fistulas, especially iatrogenic ones resulting from Caesarean sections done to relieve prolonged obstructed labour.18,19 They are thought to result from an undetected direct injury to the bladder or inadvertent inclusion of bladder tissue in closure of an incision made too low on an overstretched cervix.20 It may be associated with menouria depending on whether there was an isthmic extension.19,20 Their inaccessibility is as a result of cervical retraction following the Caesarean section.21 There is usually leakage of methylene blue dye from the upper end of the vagina as seen in the case presented. Clinical examination of this woman did not reveal the exact location as well as the size of the fistula. Radiological imaging techniques using ultrasound scan, retrograde cystography, intravenous urography and computerized tomography urography, as well as endoscopic procedures such as cystoscopy and hysteroscopy would have established the exact location as well as the size of the fistula, but these procedures were not carried out as the patient could not afford the costs. The surgery may be challenging due to limited access, fibrosis and difficulty with tissue mobilization.5 It will also imply significant expenditure on the part of the patient. They are therefore potentially good candidates for conservative management if diagnosed early. We therefore recommend that indigent women in resource-constrained settings with inaccessible fistulas be selected for conservative management without waiting for detailed endoscopic and radiological assessment, provided fistula is detected early. This approach, ifsuccessful, will improve the quality of life of these women, facilitates their rehabilitation and significantly reduce the economic burden on them.
REFERENCES
- Semere L, Nour NM. Obstetric fistula: living with incontinence and shame. Rev Obstet Gynecol 2008; 1: 193-7.
- Hurissa BF, Koricha ZB, Dadi LS. Quality of life and its predictive factors among women with obstetric fistula in Ethiopia: a cross-sectional study. Front Public Health 2022; doi: 10.33389/fpubh.2022.987659
- Sunday-Adeoye I, Daniyan ABC, Eliboh MO, Mighty-Chukwu I, Ekwedigwe KC, Nweke U, Chigbo E, Anah C. Re-integration of women who had repair of obstetric fistula – a pilot study. Ijsrm Human 2017; 8: 15-28.
- Ngongo CJ, Raassen T, Lombard L, van Roosmalen J, Weyers S, Temmerman M. delivery mode for prolonged, obstructed labour resulting in obstetric fistula: a retrospective review of 4396 women in East and Central Africa. BJOG 2020; 127: 702-7.
- Tayade S, Kumar N, Shivkumar PV. Vesicocervical fistula: a rare complication of lower segment caesarean section. IJBR 2012; 3: 221-23
- Banerjee N, Deka D, Roy KK, Takkar D. Vesicocervical fistula: an unusual presentation. Aust NZJ Obstet Gynaecol 40: 219-20.
- Federal Ministry of Health (FMOH). National strategic framework for the elimination of obstetric fistula in Nigeria 2019-2023. Abuja: Federal Ministry of Health. 2019:1-62.
- El-Azab AS, Abolella HA, Farouk M. Update on vesicovaginal fistula: a systematic review. Arab J Urol 2019; 17: 61-8.
- Waaldijk K. The immediate management of fresh obstetric fistulas. Am J Obstet Gynecol 2004; 795-9.
- Waaldijk K. Evaluation report XIV on VVF projects in Northern Nigeria and Niger. Katsina (Nigeria): Babbar Ruga Fistula Hospital. 1998; page27.
- Chinthakanan O, Sirisreetreerux P, Saraluck A. Vesicovaginal fistulas: prevalence, impact, and management challenges. Medicina 2023; 59: 1947. doi: 10/3390/medicina59111947
- Bello OO, Morhason-Bello IO, Ojengbede OA. Nigeria, a high burden state of obstetric fistula: a contextual analysis of key drivers. PAMJ 2020, 36. Doi: 10.11604/pamj.2020.36.22.22204
- Waaldijk K. The immediate surgical management of fresh obstetric fistulas with catheter and/or early closure. Int J Gynaecol Obstet 1994; 45: 11-6.
- Federal Ministry of Health (FMOH). Guidelines on urethral catheterization for prevention and management of obstetric fistula in Nigeria. 2016; 1-23.
- EngenderHealth/Fistula care. Urinary catheterization for primary and secondary prevention of obstetric fistula. Report of a consultative meeting to review and standardize the current guidelines and practices. 2013; 1-49.
- Browning A. (2004). Obstetric Fistula in Ilorin, Nigeria. PLoS Medicine, 1: e2. https://doi.org/10.1371/journal.pmed.0010002
- Daniyan ABC, Obuna JA, Daniyan OW, Yakubu EN, Ekwedigwe KC, Mbamalu SO. Predictors of late presentation for obstetric fistula repair in Abakaliki, South-East Nigeria. Afr J Reprod Health 2021; 25: 76-81.
- Azim A. Vesicocervical fistula: an uncommon presentation. Bangladesh Med J 2011; 40: 51-52.
- Wright J, Ayenachew F, Ballard KD. The changing face of obstetric fistula surgery in Ethiopia. Int J Womens Health. 2016; 8: 243-8
- Ghoniem GM, Warda HA. The management of genitourinary fistula in the third millenium. Arab J Urol 2014; 12: 97–105.
- Abodunrin ON, Daniyan ABC, Okusanya O, Ekwedigwe KC, Yakubu EN, Sunday-Adeoye I. Non-fistulous complications of prolonged obstructed labour among obstetric fistula patients in Southern Nigeria. Open J Obstet Gynecol 2019; 9: 1372