Prevalence and Determinants of Hypertension in Pregnancy (Hip) in Benue South Senatorial Zone
Ujah Innocent Achanya Otobo1, Ochejele Silas2, Onoja Michael Anthony3, Irowa Omoregie4, Ogwuche Paul Ejeh5.
1.Department of Obstetrics and Gynaecology, College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO), P.M.B 145, Otukpo, Benue State, Nigeria; 2. Department of Obstetrics and Gynaecology, College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO), P.M.B 145, Otukpo, Benue State, Nigeria; 3. Department of Haematology, College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO), P.M.B 145, Otukpo, Benue State, Nigeria; 4. Department of Obstetrics and Gynaecology, College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO), P.M.B 145, Otukpo, Benue State, Nigeria; 5. Department of Obstetrics and Gynaecology, College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO), P.M.B 145, Otukpo, Benue State, Nigeria.
ABSTRACT
Background: Hypertension in pregnancy (HIP) represent a major cause of maternal and perinatal morbidity and mortality globally, especially in Sub-Saharan Africa. There is paucity of reported study on prevalence and determinants of HIP in Benue South. Aim: To determine the prevalence and the determinants of HIP in Benue South, Nigeria. Materials and Methods: This was a descriptive cross-sectional study among 275 consenting pregnant women with HIP attending the antenatal clinics in General hospitals in 4 selected Local Government Areas (LGAs) in Benue South. Ethical clearance was obtained from the ethical committee of the committee of the Federal University of Health Sciences Otukpo (FUHSO). Data was collected using a pretested structured online questionnaire and analysed with SPSS software version 20.0. The result was presented in textual forms, charts and tables. Results: Out of 275 study participants 14 had HIP given a prevalence 5.1%. The median gestational age at diagnosis was 17 weeks. The determinants of HIP in Benue South in this study were the age groups 16-25 (aOR=0.00,CI=0.00-0.55,p-vaue=0.029) and 26-35 (aOR=0.00,CI=0.00-0.79), history of chronic hypertension (aOR=0.01, CI=0.00-0.43,p-value=0.016) and family history of HIP (aOR=0.02,CI=0.00-0.409, p-value=0.012). Conclusion: This present study demonstrated high prevalence of HIP. There is need for continuous education on the risk factors of HIP for the public and the caregivers. Policy needs to be put in place on strategies to prevent the disease as well as its adverse pregnancy outcomes
Keywords: prevalence, hypertension in pregnancy, determinants, Benue South.
Correspondence:
Innocent Achanya Otobo Ujah
Department of Obstetrics and Gynaecology,
College of Medicine, Federal University of Health Sciences, Otukpo (FUHSO),
P.M.B 145, Otukpo, Benue State, Nigeria.
+2348086575544
innocent.ujah@fuhso.edu.org/
innocentujah@ymail.com
INTRODUCTION
Hypertensive disorders represent one of the most common problems of pregnancy and causes of increased maternal and perinatal morbidity and mortality globally, particularly in developing countries like Nigeria1. The prevalence of hypertension in pregnancy (HIP) varies in the range of 1-35% around the world2. In United States of America, the prevalence of HIP was reported as at the range of 10.3%- 28.1% 3. In another study in the same country the authors reported the overall prevalence of HIP to be 8.6%, with chronic hypertension (1.9%), gestational hypertension (6.5%), and eclampsia (0.3%)4. The prevalence of HIP in Bengaluru, Southern India was at 13.9% and HIP was mostly due advance maternal age, moderate to low social support and obesity5. In China it was documented to be 7.3%; 3.3% for gestational hypertension, 4.5% for preeclampsia, 2.0% for mild preeclampsia, 0.6% for chronic hypertension (CH), and 9.6% for chronic hypertension with superimposed preeclampsia in the study conducted by Fang et al6. Estimates of prevalence of HIP and the clinical subtypes varied substantially by region and residential area, with the highest among women of Western, and Northern China women with affluent lifestyle and in women who were age 35 and above, overweight or obese6.
In a work done by Gemechu et al in sub-saharan Africa (SSA) they found out that the pooled prevalence of HIP in SSA was 8%, with preeclampsia 4.1% and gestational hypertension 4.1%, chronic hypertension (0.9%) and eclampsia (1.5%) being the less common types of hypertension in pregnancy7. It was also reported in Sokoto, Northwest of Nigeria, to be 17% and with preeclampsia 6%1. In another study in Nigeria, southwest, a prevalence of 7.2% was documented, among whom 55.9% were preeclampsia-eclampsia, 35.3% as gestational hypertension, 5.9% as chronic hypertension and 2.9% as preeclampsia superimposed on chronic hypertension 8. In a study carried out in Abuja; North central, Nigeria, the author reported that HIP was mostly determined by family history of preeclampsia, past history of preeclampsia, multifoetal gestation, and chronic hypertension9.
According to a recent report from the World Health Organization (WHO), hypertensive disorders of pregnancy (HDP) are the leading cause of maternal mortality in some African Countries 10. Globally, 2.73% of women suffer from HDP while the incidence of chronic hypertension, preeclampsia, and eclampsia are 0.29%, 2.16% and 0.28%, respectively11. HDP have contributed 14% to maternal mortality worldwide12. In addition, HDP also contribute to adverse fetal outcomes, increased the risk of preterm birth, stillbirth, small for gestational age, neonatal death and exposes the mother to an emergency cesarean section 13-15.
Evidence on the factors that determines HIP globally is limited16 and there is also paucity of reported study on prevalence of HIP in Benue State, Nigeria. This study therefore becomes necessary to determine the prevalence of HIP and its determinants in Benue South Senatorial District.
SUBJECTS AND METHODS
Study Area
Benue State is one of the North Central States in the middle belt region of Nigeria. The state occupies a landmass of 34,059 square kilometers with the geographic coordinates as longitude 7o 47’ and 10o 0’ East, Latitude 6o 25’ and 8o 8’ North, and an estimated population of 4,253,641 in the 2006 census. Benue State is inhabited predominantly by the TIV, Etulo, Idoma and Igede speaking people.
Benue State has 23 Local Governments Areas (LGA) and it’s divided into three (3) Senatorial Districts. They are Benue Northwest Senatorial District, Benue North East Senatorial District, and Benue South Senatorial District.
Benue South Senatorial District has nine (9) LGAs, namely: Ado Local Government Area, Agatu Local Government Area, Apa Local Government Area, Obi Local Government Area, Ogbadibo Local Government Area, Oju Local Government Area, Ohimini Local Government Area, Okpokwu Local Government Area and Otukpo Local Government Area.24
This study was conducted in 3 General Hospitals and 1 Missionary Hospital (Saint Mary’s Hospital Okpoga) in four Local Government Areas (LGAs) [ Otukpo, Okpoga, Ohimini, and Agatu] of Benue South Senatorial district.
Study Design
This was a health facility based descriptive cross-sectional study design.
Study Population
The study population comprises all pregnant women attending antenatal clinics in the selected health facilities.
Inclusion Criteria
All pregnant women were included in this study.
Exclusion Criteria
- Pregnant women who were critically ill were excluded from the study.
- Pregnant women who did not give consent.
Sample Size Calculation
The sample size was calculated using the formula for cross-sectional study when parameters are in normal proportion17.
N=Zn2 x PQ/E2
Where;
N= sample size
Zn2 = normal deviation for two-tailed alternative hypothesis at 5% level of significance which is 1.96.
P= Prevalence or proportion (prevalence of hypertension in pregnancy 17% from previous study in Sokoto (UDUTH), Northwest Nigeria) 1.
E= Precision or the margin of error, which is taken as 0.05(5%).
Therefore, N= (1.96)2 x17 x 83/ (5)2
=216.8
Using a non-response rate of 10% the total sample size will be N=238.
A total of 275 study participants was recruited for this study.
Sampling Technique
A purposive sampling technique was used to select the hospitals for the study, while a convenient sampling technique was used to recruit the study participants. The study participants were consecutively recruited from the selected hospitals’ antenatal clinics until the required sample size was met.
Ethical Clearance and Consent
An informed consent was obtained from each of the study participants and the ethical clearance was obtained from the Ethical Committee of Federal University of Health Sciences Otukpo (FUHSO-HREC/02/05/2023-03/05/2023).
Hypertension in Pregnancy (HIP)
HIP was defined as high blood pressure (≥140/90mmHg) in pregnancy, measured 2 times, (six hours apart by trained data collectors with or without significant proteinuria. In this study, significant proteinuria was defined as proteinuria of ++ or more (≥ 100mg/dl) on dip stick urinalysis test using a clean catch urine.
Data Collection
Data was collected from patient’s medical records, interview and measurements using pretested structured on-line questionnaire using Kobocollect by trained researcher. In addition to the biodata, other information collected include determinants of Hypertension in Pregnancy such as the literacy level and socio-economic status, history of chronic hypertension, history of preeclampsia in the previous pregnancy(ies), family history of hypertension in pregnancy, family history of chronic hypertension, parity, Age of the pregnant women and the number of fetus.
The Blood pressure of the study participants were measured while seated upright on a chair. The non-dominant arm was supported at the level of the heart on a table ensuring that no tight clothing constricts the arm. The cuff of the mercury sphygmomanometer (Accoson brand) was placed on the arm with the center of the bladder over the brachial artery. The lower edge of the cuff was placed 2-3 cm above the point of the pulsation of the brachial artery. The bladder encircled at least 80% of the arm. The systolic blood pressure was estimated by palpating the radial artery and inflating the cuff until pulsation disappears. The cuff was then deflated, and systolic blood pressure estimated. The sphygmomanometer was then inflated 30mmHg above the estimated systolic needed to occlude the pulse. A stethoscope diaphragm was then placed over the brachial artery and deflated at a rate of 2-3 mmHg/second until regular tapping sounds were heard. The systolic blood pressure was estimated at the level when the first sound was heard and diastolic blood pressure was estimated at the level when the sound muffled (Korotkoff phase IV) and these were measured to the nearest 2 mmHg.
Data Analysis
Data was analyzed with the Statistical Package for Social Sciences (SPSS) software version 20.0. Frequencies and percentages were calculated. Variables with p-value less than 0.25 in binary logistic regression analysis was subjected to multivariable logistic regression analysis to control confounders. Odds ratio with 95% confidence interval was used to examine associations between dependent and independent variables. P-value less than 0.05 was considered significant. Finally, the result was presented with tables, charts and textual forms.
Outcome Measures
- The Prevalence of hypertension in pregnancy in Benue South.
- Determinants of Hypertension in Pregnancy (HIP) in Benue South.
RESULTS
Out of a total of 275 study participants, 14 had HIP giving a prevalence of 5.1%.
Table 1 shows the sociodemographic characteristics of the study participants. The mean age was 27.47±6.43. Majority of the study participants were in the age group 26-35(58.5%), Idoma (86.5%), Christians 251 (91.3%) and with secondary level of education113 (41.1%). Most of the study participants were of small-scale business 98(35.6%) and monthly income of < 30,000 (68.7%). Agatu local Government Area account for the majority of the study population of 100(36.4%).
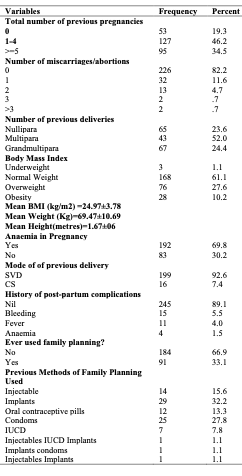
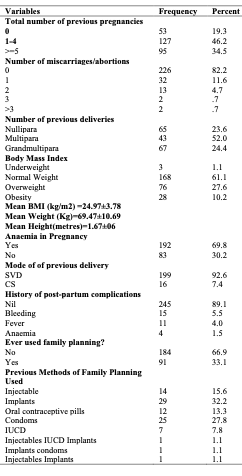
Table 2 shows the clinical characteristics of the study participants. Most of the study participants with previous pregnancies, miscarriages, and previous deliveries belongs to 1-4 group (46.2%), no miscarriages (82.2%), and multipara 143 (52.0%) respectively. Majority of the study participants had anaemia 192(69.8%). Most of the study participants, 199 (92.6%) had spontaneous vaginal delivery (SVD). Majority, 184 (66.9%) had not used contraception previously while the most frequently used method of contraception was implants 29(32.2%) among the study participants.
Table 3 shows the laboratory characteristics of study participants. The majority, 257(93.5%) of the study participants at booking had negative urinalysis for protein, glucose 271(98.5%), nitrites 271(98.5%), and blood 275 (100%). Most of the study participants at diagnosis had urinalysis negative for protein 261(94.9%), glucose 273(99.3%), nitrites274 (99.6%), and blood 275(100%). For those with proteinuria, 11(4.0%) had one plus (1+) of protein and 13 (4.7%) had mild degree of proteinuria
Table 1 Sociodemographic Characteristics of Study Participants (n=275)
|
Variables
|
Frequency
|
Percent
|
|
Age (in years)
|
|
|
|
16-25
|
90
|
32.7
|
|
26-35
|
161
|
58.5
|
|
36-45
|
15
|
5.5
|
|
46-55
|
9
|
3.3
|
|
Mean Age =27.47±6.43
|
|
|
|
Tribe
|
|
|
|
Idoma
|
238
|
86.5
|
|
Tiv
|
8
|
2.9
|
|
Igbo
|
15
|
5.5
|
|
Hausa
|
9
|
3.3
|
|
Yoruba
|
2
|
.7
|
|
Others
|
3
|
1.1
|
|
Religion
|
|
|
|
Christianity
|
251
|
91.3
|
|
Islam
|
24
|
8.7
|
|
Level of Education
|
|
|
|
Tertiary
|
74
|
26.9
|
|
Secondary
|
113
|
41.1
|
|
Primary
|
57
|
20.7
|
|
None
|
31
|
11.3
|
|
Occupation
|
|
|
|
Small scale business
|
98
|
35.6
|
|
Large scale business
|
11
|
4.0
|
|
Junior civil servant
|
40
|
14.5
|
|
Student/full time housewife
|
67
|
24.4
|
|
Farming
|
59
|
21.5
|
|
Income per Month
|
|
|
|
≤30000
|
189
|
68.7
|
|
30001-50000
|
18
|
6.5
|
|
50001-80000
|
44
|
16.0
|
|
80001-110000
|
17
|
6.2
|
|
>110000
|
7
|
2.5
|
|
Median Income=20,000
|
|
|
|
Local Government Areas
|
|
|
|
Okpokwu
|
67
|
24.4
|
|
Agatu
|
100
|
36.4
|
|
Otukpo
|
59
|
21.5
|
|
Ohimini
|
49
|
17.8
|
|
Hospitals
|
|
|
|
ST Mary's Hospital Okpoga
|
67
|
24.4
|
|
GH Otukpo
|
59
|
21.5
|
|
GH Idekpa
|
49
|
17.8
|
|
GH Obagaji
|
46
|
16.7
|
|
CHC Obagaji
|
54
|
19.6
|
Table 4 shows the sociodemographic determinants of hypertension in pregnancy. The age (Fishers Exact Test= 12.774, p-value=0.003), LGAs (Fishers Exact Test=19.359, p-value<0.001, occupation (Fishers Exact Test= 9.275, p-value=0.032) and monthly income (Fishers Exact Test= 14.600, p-value=0.003) were statistically significant with p-value < 0.05 on bivariate analysis.
Table 2 Clinical Characteristics of Study Participants(n=275)

Table 5 shows the clinical determinants of hypertension in pregnancy. The total number of previous pregnancies (Fishers Exact Test= 8.625, p-value=0.008), BMI (Fishers Exact Test= 11.533, p-value=0.007), history of chronic hypertension ( Fishers Exact Test= 17.912, p-value=0.000), history of preeclampsia( Fishers Exact Test= 31.778, p-value<0.001), family history of hypertension in pregnancy( Fishers Exact Test= 18.621, p-value<0.001) and family history of chronic hypertension( Fishers Exact Test=
5.652, p-value=0.017) were statistically significant on bivariate analysis (p-value <0.05).
Table 6 shows multiple logistic regression analysis of the determinants of hypertension in pregnancy. Only the
Table 3 Laboratory Characteristics of Study Participants (n=275)

study participants in the age groups 16-25 (aOR=0.00, CI=0.00-0.55,p-vaue=0.029) and 26-35 (aOR=0.00,CI=0.00-0.79), history of chronic hypertension (aOR=0.01, CI=0.00-0.43,p-value=0.016) and family history of hypertension in pregnancy (aOR=0.02,CI=0.00-0.409, p-value=0.012) were statistically significant.

Figure 1: Prevalence of Hypertension in pregnancy in Benue South Senatorial District.

Figure 2: Severity of hypertension in pregnancy in Benue South. Majority, 12(85.7%), had mild HIP.
Table 4 Determinants (sociodemographic risk factors) of Hypertension in Pregnancy

*p-value<0.05
Table 5 Determinants (clinical risk factors) of Hypertension in Pregnancy

*p-value<0.05
Table 6 Multivariate logistic analysis of the determinants of Hypertension in pregnancy
Note: *p-value <0.05, Omnibus Tests=77.77, df= 17, p=0.000, Hosmer and Lemeshow Test χ2=2.89, p=0.894, Nagelkerke R2=0.743
DISCUSSION
To the best of our knowledge, this is the first base-line study to characterize hypertension in Pregnancy in Benue South Senatorial District of Nigeria, aimed at generating data among common diseases in this part of Nigeria.
The prevalence of hypertension in pregnancy in the study was 5.1%. This suggests a high burden of the disease in Benue South but consistent with the global prevalence range of 5-10% of all pregnancies 2, 6,18. The prevalence of hypertension in pregnancy in this study is also similar to the pooled prevalence of 8 % in the Sub-Saharan Africa which is high when compared to other regions of the world 7. Millogo et al in Burkina Faso reported a similar prevalence rate of 9.6% 19.
In a study in Ekiti, Nigeria by Oladele et al, the prevalence of HIP was 7.2% which was in keeping with the findings in our study, however in a similar study by Singh et al in Sokoto and Ayogu et al in Abuja, Nigeria, they reported a higher prevalence of HIP of 17% and 19.4 respectively 1,8,9. This perhaps, shows regional variations in the burden of hypertension in pregnancy in Nigeria. The higher prevalence in these studies may due to the differences in the study centres, because these studies with higher prevalence were conducted in tertiary hospitals which are all referral centres, where majority of the high-risk pregnancies are managed when compared with the secondary healthcare facilities where this current study were carried out1,9. The finding from this study also differs from studies of Walle et al and Johnson et al in Ethiopia with a prevalence of 16.8% and 22.2% respectively14,20.This may be due to the large sample size used in their study when compared to our study. High prevalence of 13.9% was seen in a similar study in Bengaluru by Nath et al, this may be attributable to the large sample size in their study5. The high burden of hypertension in pregnancy is concomitantly associated with significant adverse maternal and perinatal outcomes as shown in previous studies by Endeshaw et al, Nakimuli et al and Browne et al 13,15,18. Hypertension in pregnancy is the second leading cause of maternal mortality worldwide 18. Therefore, government of the various tiers in collaboration with non-governmental agencies, both local and international should develop policies that will help to prevent and control hypertension in pregnancy in order to mitigate the adverse pregnancy outcomes associated with the high burden of the disease.
The determinants of hypertension in pregnancy in Benue South as was demonstrated in this study include age group (16-25, and 26-35), history of chronic hypertension and family history of hypertension. Other studies also demonstrated similar risk factors among other determinants of hypertension in pregnancy 9,20-22. Belayhun et al in a similar study found rural residents, illiterate, history of pregnancy induced hypertension, history of kidney disease and family history of hypertension as the risk factors that are significantly associated with HIP 21. Ayogu et al associated family history of preeclampsia, previous history of preeclampsia, multiple gestation, chronic hypertension and diabetes as determinants of HIP 9. Walle et al in their study found family history of hypertension, and alcohol intake drug pregnancy as risk factors associated with HIP 20. Also, Tesfa et al identified maternal age ≥ 35, twin pregnancy, previous history of preeclampsia, family history of hypertension, family history of diabetes mellitus, BMI ≥ 25, alcohol consumption, urinary tract infection, lack of nutritional counselling during antenatal period, lack of fruits and vegetable consumption as the determinants of HIP 22. However, this study differs from the study by Singh et al 1. They found previous history of preeclampsia, multiple gestation, gestational diabetes, obesity to be significantly associated with HIP among the study population. Also, Nath et al identified employed outside the house, obese respondents, higher maternal age and lower socioeconomic status as the determinants of HIP 5. This differs from the findings of this present study. Similarly, Zhao et al differs found living in rural areas, older age, lower education, history of caesarean section gestational diabetes and high BMI in the first trimester 23. Thus, there is need for continuous education on the determinants of HIP to the public, health care giver, and policy makers to strategize ways to prevent and control the risk factors of the disease as well as adverse pregnancy outcomes.
The strength of this study was the multiple secondary health facilities used for this study as against to previous studies which were conducted in tertiary centres and using single centre for the study. Therefore, findings from this study can be inferred to be representative of centres of similar characteristics which could be extrapolated to population with similar qualities. The study findings could be foundational in designing advocacy and awareness creation policies to prevent and control risk factors associated with hypertension in pregnancy and provide treatment options to help clinicians effectively treat this condition so as to prevent adverse pregnancy outcomes. The limitation of the study was that it was a descriptive and cross-sectional, therefore a casual and effect relationship cannot be established using this study design.
In conclusion, the study has provided a background data on hypertension in pregnancy showing a high prevalence (5.1%) of HIP and its determinants of HIP in Benue south Senatorial District of Benue State with age group of 16-25, and 26-35, history of chronic hypertension and family history of hypertension. Therefore, there is the need to develop preventive measures to control these factors in order to reduce the burden of this disease as well as its associated adverse pregnancy outcomes in Benue South Senatorial District of Benue State. It is recommended that a detailed longitudinal study on HIP in Benue south as well as determine the associated adverse pregnancy outcomes.
REFERENCES
- Singh S, Ahmed EB, Egondu SC, Ikechukwu NE. Hypertensive disorders in pregnancy among pregnant women in a Nigerian Teaching Hospital. Niger Med J. 2014 ;55(5):384- 8.
- Sutton ALM, Harper LM, Tita ATN. Hypertensive Disorders in Pregnancy. Obstet Gynecol Clin North Am. 2018 ;45(2):333-347.
- Bello NA, Zhou H, Cheetham TC, Miller E, Getahun DT, Fassett MJ, Reynolds K. Prevalence of Hypertension Among Pregnant Women When Using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines and Association with Maternal and Fetal Outcomes. JAMA Netw Open. 2021 Mar 1;4(3):e213808.
- Butwick AJ, Druzin ML, Shaw GM, Guo N. Evaluation of US State-Level Variation in Hypertensive Disorders of Pregnancy. JAMA Netw Open. 2020 ;3(10):e2018741.
- .Nath A, Sheeba B, Sisira R, Metgud CS. Prevalence of hypertension in pregnancy and its associated factors among women attending antenatal clinics in Bengaluru. J Family Med PrimCare. 2021;10(4):1621-1627.
- Li F, Qin J, Zhang S, Chen L. Prevalence of hypertensive disorders in pregnancy in China: A systematic review and meta-analysis. Pregnancy Hypertens. 2021; 24:13-21.
- Gemechu KS, Assefa N, Mengistie B. Prevalence of hypertensive disorders of pregnancy andpregnancy outcomes in Sub-Saharan Africa: A systematic review and meta-analysis. Womens Health (Lond). 2020 Jan-Dec; 16:1745506520973105. doi: 10.1177/1745506520973105.
- Oladele FC, Charles-Davies MA, Ojengbede OA, Agbedana EO. Prevalence of hypertensivedisorders in pregnant Nigerian and their related factors. Afri. J. Med. Med. Sci.2018; 4: 297-305
- Ayogu ME, Akaba GO, Offiong RA, Adewole ND, Ekele BA. Risk factors for hypertensivedisorders of pregnancy in Abuja, Nigeria: A prospective case‑control study. TropJObstet Gynaecol, 2020;37(1):46-52.
- Fokom-Domgue J, Noubiap JJ. Diagnosis of hypertensive disorders of pregnancy in sub Saharan Africa: a poorly assessed but increasingly important issue. J Clin Hypertens (Greenwich). 2015;17(1):70-3.
- Raphael, O., John, O. O., Sandra, U. I., & Sunday, A. C. (2018). Assessment of Borehole Water Quality Consumed in Otukpo and Its Environs. International Journal of Ecological Science and Environmental Engineering, 5(3), 71–78. http://www.aascit.org/journal/ijesee
- Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, Gülmezoglu AM, TemmermanM, Alkema L. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014 Jun;2(6):e323-33.
- Nakimuli A, Nakubulwa S, Kakaire O, Osinde MO, Mbalinda SN, Kakande N, et al. The burden of maternal morbidity and mortality attributable to hypertensive disorders in pregnancy: a prospective cohort study from Uganda. BMC Pregnancy Childbirth. 2016 4;16:205.
- Johnson KM, Zash R, Haviland MJ, Hacker MR, Luckett R, Diseko M, et al. Hypertensive disease in pregnancy in Botswana: Prevalence and impact on perinatal outcomes. Pregnancy Hypertens. 2016;6(4):418-422.
- Browne JL, Vissers KM, Antwi E, Srofenyoh EK, Van der Linden EL, Agyepong IA, et al. Perinatal outcomes after hypertensive disorders in pregnancy in a low resource setting. TropMed Int Health. 2015 Dec;20(12):1778-86.
- Meazaw MW, Chojenta C, Muluneh MD, Loxton D. Factors associated with hypertensive disorders of pregnancy in sub-Saharan Africa: A systematic and meta-analysis. PLoS One. 2020 Aug 19;15(8): e0237476.
- Hanga A, Johargy A. Design and Determination of The Sample Size in Medical Research. IOSR Journal of Dental and Medical Sciences, 2014; 13(5): 21-31.
- Endeshaw G, Berhan Y. Perinatal Outcome in Women with Hypertensive Disorders of Pregnancy: A Retrospective Cohort Study. Int Sch Res Notices. 2015 Jan 8; 2015:208043. doi:10.1155/2015/208043.
- Millogo GRC, Yaméogo RA, Mandi DG, Sompougdou C, Naibé DT, Kologo kJ et al. Hypertension in Pregnancy at the Teaching Hospital of Yalgado Ouédraogo, Burkina Faso. J Hypertens 2015;4: 199. http //dx.doi:10.4172/2167-1095.1000199
- Walle TA, Azagew AW. Hypertensive disorder of pregnancy prevalence and associated factors among pregnant women attending antenatal care at Gondar Town Health Institutions,North West Ethiopia 2017. Pregnancy Hypertension, 2019; 16: 79-84.
- Belayhun Y, Kassa Y, Mekonnen N, Binu W, Tenga M, Duko B. Determinants of PregnancyInduced Hypertension among Mothers Attending Public Hospitals in Wolaita Zone,South Ethiopia: Findings from Unmatched Case-Control Study. Int J Hypertens. 2021Oct 28;2021:6947499.
- Tesfa E, Nibret E, Gizaw ST, Zenebe Y, Mekonnen Z, Assefa
S, et al. Prevalence and determinants of hypertensive disorders of pregnancy in Ethiopia: A systematic reviewandmeta-analysis. PLoSONE, 2020; 15(9): e0239048.
- Zhao W, Di J, Haung A, Yang Q,Hu H. Incidence and risk factors of hypertensive disorders of pregnancy 8 provinces, China, 2014-2018.CCDC Weekly, 2021; 3(22): 476-482.
Acknowledgement:
We acknowledge the financial support from Tetfund under the Institutional Based Research (IBR) Grant. We appreciate the Hospitals and Clinics where the research was conducted. We thank all the patients who volunteered tom participate in the research study.