INTRODUCTION
Preterm (or premature) prelabour rupture of fetal membranes (PPROM) is a significant contributor to preterm birth and a leading cause of perinatal morbidity and mortality worldwide. 1,2 In Nigeria, the reported incidence of preterm birth varies between 5.8% and 11.1%.3,4 Also, preterm babies account for 40-60% of all perinatal deaths.3 To reduce perinatal mortality requires understanding the clinical characteristics and risk factors of PPROM.
Rupture of fetal membranes (ROM) is a normal component during labour, usually occurring after the onset of established uterine contractions.1However, fetal membrane rupture may occur at any time in second or third trimesters of pregnancy. Preterm rupture of membranes is the rupture of fetal membranes before 37weeks of pregnancy. Prelabour rupture of fetal membranes however is the spontaneous rupture of fetal membranes prior to the onset of labour. 1,5
Generally, prelabour rupture of membranes occurs in about 3 – 6% of all pregnancies and approximately 60-80% of cases of prelabour rupture of membranes occur at term. 1,5 In Nigeria, incidences of 0.94% and 3.3% have been reported in different studies6,7. While the aetiology of PPROM is multifactorial, intrauterine infection is the most common risk factor. The proposed hypotheses for fetal membrane rupture involves a progressive decrease in the collagen content of the amnion in the later part of pregnancy. This is believed to account for the spontaneous rupture of membranes during labour, which is a physiological event. However, whether the same applies to PPROM is not fully established 8. It is hypothesised that obstetric infections or de novo inflammatory processes, are triggers for the progressive disruption of collagen content in fetal membranes.9
Risk factors associated with ROM include conditions like bacterial vaginosis, cervical weakness, abnormal lie, polyhydramnios and multiple pregnancy as well as socio-demographic characteristics like low socio-economic status, black race, cigarette smoking and previous history. 1,5
More than 90% of patients presenting with PPROM will provide a clinical feature of fluid leakage from the vagina. 1,5 Occasionally, patients will present with history of perineal dampness or an isolated loss of fluid. Such women would require additional tests to confirm the diagnosis. It is important to verify the gestational age of the indexed pregnancy because this information will directly affect subsequent management.1 Obstetric ultrasound assessment is useful for pregnancy dating, to ascertain the presence of oligohydramnios and measure the biophysical profile 10,11. A speculum examination should be done to confirm the flow of fluid from the cervical os, and ascertain the presence or otherwise, of cervical dilatation and effacement. Digital vaginal examination should be avoided unless the patient is having uterine contractions or suspected to be in established labour. Digital vaginal examination increases the risk of infectious morbidities. 1,5 The presence of amniotic fluid can be further ascertained by ferning test, nitrazine test, amnisure and assays for specific molecules which are present in high concentrations in the amniotic fluid. 1,5 The mode of management of PPROM depends on gestational age and mode of presentation of the patient.1
Gestational age should be ascertained by reliable last menstrual period, or preferably by early ultrasound scan assessment where available. PPROM is far more challenging to manage than fetal membrane rupture at term as prematurity must be weighed against maternal and perinatal infectious morbidities. Patient should be counseled with regards to neonatal survival as this is contingent on the expertise available for neonatal care. The Neonatologist should be involved in the management of these patients from the start. Obstetric care should take place in a facility with neonatal unit equipped to cater for preterm babies. 1,5 In women between 34 to 36 weeks of pregnancy, where fetal lung maturity is generally expected, immediate induction of labour is the management line of choice.10 In cases between 28 to 33weeks, conservative management is the rule in the absence of chorioamnionitis or any threat to the fetomaternal wellbeing.1,10 The use of antibiotics and corticosteroid have been shown to improve fetomaternal outcome.1,5,10
The implication of adequate care for women with PPROM and their neonates is huge in socio-economic, medical and psychological terms. Studies like this may provide clinical evidence upon which to base advice to women with PPROM, and identify treatment strategies. It is for these reasons that studies like this is important. Our aim is to determine the prevalence and feto-maternal outcome of PPROM in UNIMEDTH Complex, Ondo over a 5-year period.
Aim And Objectives
AIM: To review cases of preterm prelabour rupture of membrane at the UNIMEDTH Complex, Ondo, over a 5-year period.
Objectives
- To determine the prevalence of PPROM at the UNIMEDTH Complex, Ondo
- To identify their socio-demographic and clinical characteristics
- To evaluate associated maternal and perinatal outcomes
MATERIALS AND METHODS
Study Setting
The Department of Obstetrics and Gynaecology of the state government-owned University of Medical Sciences Teaching Hospital Complex, Ondo was established in August 2018. The structure housing the Department was formerly known as the Mother and Child Hospital Ondo which, from inception in November 2012 till 2015, ran a free maternity care service. However, subsidized fee-paying services were introduced from 2016 till 2018. Our facility continues to serve the obstetric population majorly from the central and southern senatorial districts of Ondo state, representing roughly two-thirds of the total population.
Methods
This study is a retrospective review of patients who presented with preterm prelabour rupture of membrane and were managed at UNIMEDTH Complex, Ondo, Nigeria from 1st January 2013 to 31st December 2017. Over this period, all patients coded as PROM by our Health Information unit were identified. A total of 370 patient files were so coded. These medical histories were retrieved. These records were reviewed by one of the authors and data extracted according to pro-forma designed for this purpose. Labour ward records were also perused for relevant data concerning these patients. A total of 352 patients were confirmed as PPROM from these clinical records and were of gestational ages between 28 weeks to less than 37 completed weeks. Gestational ages were based on recorded, reliable dates of the last menstrual period provided. Occasionally, early ultrasound assessment was used, where available. Labour room records also served as sources of confirmation of the PPROM diagnosis. The protocol for management of PPROM in our institution included the use of steroids given intramuscularly in prescribed international doses over 48hour period and antibiotic therapy usually erythromycin. Tocolysis was not practised.
Ethical Consideration and Data
The study involved the use of anonymised data, for which the UNIMEDTH gave consent. The following data was extracted: maternal age, parity, educational status, occupation, marital status, gestational age at presentation, mode of delivery, fetomaternal outcomes like Apgar scores and birth weight and mode of delivery. Complications arising from delivery and neonatal care were obtained from Labour room record. Neonatal data were obtained from the Neonatal Intensive Care Unit (NICU) record. The total number of deliveries during the period of study was obtained from the delivery register and confirmed by our Health Information Unit. The data collected were collated in proforma forms designed for this purpose and inputted and analyzed with Statistical Package for Social Sciences (SPSS) (Windows version 23) computer software.
RESULTS
A total of 352 women with the admission diagnosis of preterm prelabour rupture of membranes were seen at the UNIMEDTH Ondo over the period of this study. The total number of delivery during this time, as provided by our Health Information unit, was 13,425 births. The incidence of PPROM was 2.6%. The socio-demographic data of the women are as shown in Table 1. The mean age of the subjects was 30.02 ± 5.26 years while the 30-34 years age group had a frequency of 112 representing 31.8%.
Parameters of the obstetric history of the women are shown in Table 2. Majority (68.5%) of the women were not registered for obstetric care at our facility. Only 31.5% of the women were booked for antenatal care and delivery at our facility. Majority of presenting parturient were of low parity (<2) accounting for 79.6% of cases, and 48.9% of the women had a previous history of miscarriage. There were 12 women (3.4%) with multiple pregnancies. Mean Gestational Age at presentation was (32.12 ± 2.41) weeks. Women in the gestational age bracket of 31-33weeks were highest in number accounting for 127(36.1%) of the cases.
Table 1. Maternal Socio-Demographic Characteristics

Table 2. Obstetric History of Patients.

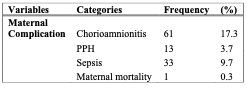
Table 3: Maternal Outcome

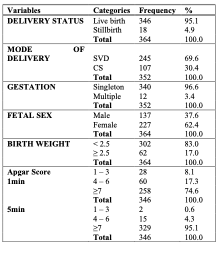
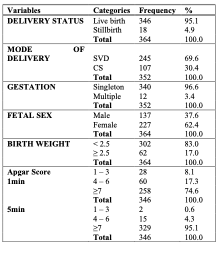
The maternal outcome is shown in Table 3. Clinical evidence of chorioamnionitis was present in 17.3% of the women and 9.7% had puerperal sepsis. One woman (0.3%) died due to puerperal sepsis. The fetal outcome is presented in Table 4. Majority of the women (67.3%) delivered vaginally while 32.7% had Caesarean section. There was a total of 364 births, 346 (95.1%) of which were live births while 18(4.9%) were still births. Birth weight less than 2.5kg was observed in 302 neonates which represents 83% of all births. The first minute Apgar score was less than seven in 88(25.4%) but only 17(4.9%) of the live neonates had five minutes Apgar score < 7.
The neonatal outcome is shown in Table 5. Most, (72 %), of the neonates were admitted to the neonatal intensive care ward. Of those that required NICU admission, 68.7 % were on admission for up to 1 week while 21.3 % were on admission for between 1-4 weeks. There were 35 neonatal deaths, 20 of which occurred within the first week of life. The perinatal mortality represents 10.4% of all deliveries.
Table 4. Fetal Outcome
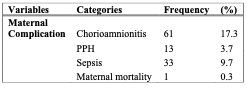
Table 5. Neonatal Outcome. (Nicu: Neoatal Intensive Care Unit)
DISCUSSION
There were 13,425 deliveries over the period of this study with 352 women clinically confirmed to have preterm prelabour rupture of membranes. The incidence of preterm prelabour rupture of membranes was 2.6%. This incidence is comparable to 2.5% found in Enugu, Nigeria by Obi et al and 3.1 % found by Hackenhaar et al in a similar study in Brazil.[7,12]. Okeke and other workers also found an incidence of 3.3% in a tertiary hospital in Nigeria.13 Unbooked patients accounted for over half of the women in this series. This finding probably reflects the poor attitude of our women towards antenatal care and enrolment. Despite free obstetric services for most of the period of this study, 68.5% of women failed to register for obstetric care. The alarming and emergency nature of PPROM apparently forced them to seek specialist attention. Our rate of 68.5% is higher than 50.2% by Okunade et al 14 and 20.7% by Zini et al15 in southern Nigerian population. Zini and co-workers confirmed that the unbooked status showed some association with preterm birth. The mean age of the women in our series is 30.02 ± 5.26 years, a figure comparable to 31.3±5.0years found by Okunade et al.14 The 26 –30 years age group had the highest frequency, accounting for 33% of cases. Okunade and co-workers however, had an older demographic with the age group 30-34years having the highest frequency of 39.4%. The nulliparous women in this series accounted for the highest number of cases at 52.6%, a figure higher than the 42.3% recorded by Noor and co-workers in a Pakistani study.16 Most of the women in our study were of low parity, which is similar to the finding of Obi and co-workers. However, 75.65% of patients in the series by Hossain et al17 were primipara. It would appear that younger women of low parity are the identified risk group in many series. The presentation was cephalic in about 77.5% of cases and breech in about 19.5%. The fact that most babies are preterm and the increased rates of multiple pregnancies in the cohort, accounted for this finding.
About half (49%) of the women had a history of previous miscarriage whether voluntary or spontaneous. This agrees with the finding of Obi et al.7 Previous miscarriage may lead to cervical weakness, a known risk factor for PPROM. This finding would suggest the need for sonographic evaluation of cervical length at specified gestational ages, in pregnant Nigerian women. The mean gestational age at delivery in this series, is 32.12 ±2.41 weeks. This is in consonance with the figure of 32.7±2.4weeks by Okunade and co-workers in the same geographical area in Nigeria. Noor and others, in Pakistan, found that women with PPROM delivered at significantly lower gestational ages (31-35) compared with control women with preterm labour.20 Hossain and others also reported a mean gestational age of 32.34weeks at delivery for women in Pakistan.17 The mean gestational age at delivery appear to vary from one geographical area to another, probably due to recruitment criteria and the socio-demographic characteristics of the population. The highest number of cases in our series were between 31-33 weeks gestational age, which is in contrast to the findings of Obi et al in which 28-30 weeks gestational age had the highest number of patients. 7
Cesarean section was the mode of delivery in 33% of patients in this study, a figure less than the 37.1% rate obtained by Yu and co-workers19in a tertiary centre in China and 44.35% by Hossain and others.17 The higher figure reported by Yu and co-workers may be explained by their recruitment of women below 34weeks gestation. Despite similar mean gestational age at delivery of 32.34weeks, the caesarean rate of 44.35% is markedly higher than our figure of 33%. It would appear that other factors underscore the decision to deliver abdominally. Okunade and others reported a Caesarean rate of 49.3% despite having the highest percentage of their subjects between 34week and 36weeks gestation. They averred that the threshold for Caesarian delivery was unnecessarily low in their centre. Noor and co-workers, in their comparative prospective study, reported a Caesarian section rate of 14%20, a figure that bucks the trend of high Caesarean rates in many series. Their study sample size of 85 PPROM patients were compared with equal number of women with preterm labour.
Their reported Caesarean section rate could not be explained on the basis of mean gestational age at delivery nor by the proportion of low birthweight babies. About 62% of the neonates in our series were female while 38% were male. Eighty three percent (83%) neonates in this series had birth weights less than 2.5kg. Our figure is higher than 79.1%% found by Okunade in Lagos, Nigeria, and 62.3% reported by Noor and co-workers, from Pakistan.14,20 The proportion of low-birth-weight babies delivered may be due to socio-demographic factors of the parturient and their reported mean gestational age at delivery. One-minute Apgar score less than 7 was reported in about 25% of our neonates, a figure that underscores the high-risk category of babies born following PPROM. However, Apgar scores less than 7 were observed in 5% of the neonates at 5 minutes. This marked improvement in the physical evaluation of these newborn babies, attests to the effectiveness of neonatal resuscitation at our centre. Comparatively, Sultana and co-workers found that 54.8% and 30.6% of neonates in their series, had Apgar scores <7 at 1 and 5-minute scores respectively.[21]Stillbirth rate of 5% was recorded in this study, a figure in synchrony with 5.88% found by Noor et al.16. Seventy two percent (72%) of the neonates required neonatal ward admission, a figure similar to 72.5% reported by Okunade and co-workers and 72.9% by Yu and colleagues.14,19 Our neonatal ward admission appears high despite the low figure of 5% neonates with Apgar scores less than 7 at 5minutes. This observation is probably explained by the high proportion (83%) of low birth weight babies born in our series. There is strong possibility that indications for neonatal ward admission would vary between institutions as a result of proportion of low birth weight neonates, prevalent neonatal complications and staff complement available. We recorded 18 stillbirths, and one severe case of severe puerperal sepsis leading to maternal death. These events are probably due to delay in seeking medical specialist attention. About 69% of neonates admitted to our intensive care unit stayed for up to one week, 21% from one week but up to 4 weeks, while 10% were on admission for more than 4 weeks.
There were 35 neonatal deaths, a figure representing 10.1% of live births, 20 of which were early neonatal deaths. From this study, the perinatal mortality was 10.4%, a figure lesser than 13% recorded by Noor et al and 52% found by Obi et al.7,16 The high perinatal mortality recorded by Obi and colleagues was most likely due to the high proportion of women with gestational ages between 28 to 30weeks gestation in their series. Another explanation may be the quality of neonatal intensive care services available at that time in their institution. Sixty-one (17.3%) of the patients had clinical evidence of chorioamnionitis, 13(3.7%) had postpartum hemorrhage, and 33(9.4%) had puerperal sepsis. One(0.3%) maternal death was recorded which was lesser than 0.6% found by Obi et al.7 The comparatively low complication rates recorded in our series can be linked to the protocol of administration of antibiotics, corticosteroids and clinical vigilance to identify complications and treat them promptly.
CONCLUSION
The incidence of Preterm pre-labour rupture of membranes at our facility is 2.6%. Younger women of low parity are the modal at risk group, majority of whom were not registered for antenatal care at our facility. The mean gestational age at delivery was 32.12±2.14weeks. This factor, combined with possible delay at seeking specialist treatment, contributed to the high maternal morbidity, and the high perinatal and neonatal mortality in our series. Majority of the neonates required neonatal intensive care. The increased perinatal and neonatal deaths make the availability of efficient neonatal care services mandatory. Obstetricians must be on alert for increased maternal morbidities, especially chorioamnionitis and puerperal sepsis.
Recommendations
- Continued researches to identify local and peculiar socio-demographic factors associated with PPROM in the country.
- Consistent advocacy to ensure early registration for antenatal care. Pregnant women should be alerted through media to recognize both the clinical signs and the seriousness of PPROM. Women with PPROM must be advised to present early in hospital for the prompt management of this condition.
- Delivery of these high risk women in centres equipped with Neonatal Intensive Care Units. Prompt care of these preterm neonates would reduce the morbidity and mortality associated with PPROM.
Conflict of Interest: There are no conflict of interest.
REFERENCES
- Mercer, B. Premature Rupture of Membranes. Glob. libr. women’s med; (ISSN:1756-2228) 2008; DOI 10.3843/GLOWM. 10120
- Goldenberg RL, Culhane JF, Lams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008; 371: 75-84.
- Akintayo AA, Awoleke JO, Ogundare EO, Olatunya OS, Aduloju OP. Preterm births in a Resource constrained setting: socio-biological risk factors and perinatal outcomes. Ghana Medical Journal. 2015; 49(4), 251-256
- Ezechi OC, David AN, Gab-Okafor CV, Ohwolo H, Oladele DA, Kalejaiye OO et al. Incidence and socio-biologic risk factors for spontaneous preterm birth in HIV positive Nigerian women. BMC Pregnancy Childbirth 2012; 12:93
- Medina TM, and Ashley Hill D. Preterm Premature Rupture of Membranes: Diagnosis and Management. Am. Fam. Physician 2006; 73(4), 659-664
- Dare FO, Ademowore AS, Ogunniyi SO. Experience with 159 cases of premature rupture of foetal membranes in Ile-Ife, Nigeria. Trop Doct. 1989; 19(4), 160-162
- Obi SN and Ozumba BC. Preterm premature rupture of fetal membranes: The dilemma of management in a developing nation. J. Obstet Gynaecol. 2007; 27(1): 37-40.
- Steer P, Flint C. Preterm labour and premature rupture of membranes. BMJ. 1999 April 17; 318(7190): 1059-1062.
- Bendon RW, Faye-Petersen O, Pavlova Z, Qureshi F, Mercer B, Miodovnik M et al. Fetal membrane histology in preterm premature rupture of membranes: comparison to controls and between antibiotic and placebo treatment. Paediatr Dev Pathol 1999; 2: 552-558.
- Ioannis Tsakiridis, Apostolos Mamopoulos, Eleni-Markella Chalkia-Prapa, Apostolos Athanasiadis and Themistoklis Dagklis. Preterm Premature Rupture of Membranes: A Review of 3 National Guidelines. Obstetrical and Gynecological Survey 2018: 73(6), 368-375.
- Royal College of Obstetricians and Gynaecologists. Preterm prelabour rupture of membranes. Green Top Guideline No.44. London, RCOG; 2010.
- Hackenhaar AA, Albernaz EP, da Fonseca TM. Preterm rupture of fetal membranes: Association with socio-demographic factors and maternal genitourinary infections. J.Pediatr (Rio J). 2014 Mar-Apr; 90(2): 197-202.
- Okeke TC, Enwereji JO, Okoro OS, Adiri CO, Ezugwu EC, Agu PU. The incidence and management outcome of Preterm Premature Rupture of Membranes (PPROM) in a Tertiary Hospital in Nigeria. American Journal of Clinical Medicine Research. 2014; 2(1), 14-17. https://doi.org/10.12691/ajmr-2-1-4
- Okunade KS, Ajepe A, Omisakin SI, Hakeem-Adeyemi FM, Sekumade A, Moses OE. A Review of Fetomaternal Outcome of Preterm Prelabour Rupture of Membranes in a Tertiary Hospital in Lagos, South-west Nigeria. Nig Hosp Pract 2015; 16(1-3): 13-18.
- Zini ME, and Omo-Aghoja LO. Clinical and socio-demographic correlates of preterm deliveries in two tertiary hospitals in southern Nigeria. Ghana Med J. 2019; 53(1): 20-28. http://dx.doi.org/10.4314/gmj.v53il.4
- Noor S, Nazar AF, Bashir R, Sultana R. Prevalence of PPROM and its outcome. Journal of Ayub Medical College, Abbottabad 2007; 19(4), 14-17.
- Hossain S, Sultana SS, Biswas JR, Noor MS, Farzana S. Clinical Profile and Feto-Maternal Outcome of Preterm Prelabour Rupture of the Membrane in a Tertiary Level Hospital. KYAMC Journal 2021; 12, (3): 166-171.
- Akter S, Ather R, Rashid M. Preterm rupture of fetal membranes and Fetomaternal outcome: an observational study. Journal of Bangladesh College of Physicians and Surgeons. 2010 Jan Vol. 28, No 1
- Yu H, Wang X, Gao H, You Y, Xing A. Perinatal outcomes of pregnancies complicated by preterm premature rupture of membranes before 34weeks of gestation in a tertiary center in China: A retrospective review. BioScience Trends 2015; 9(1): 35-41.
- Noor S, Fawwad A, Shahzad H, Sultana R, Bashir R. Foetomaternal outcome in Patients with or without Premature Rupture of membranes. J Ayub Med Coll Abbottabad 2010; 22(1).
- Sultana S, Ishtiaq S, Malik U, Akhai AZ, Nadeem K. Maternal and perinatal outcome in preterm prelabor rupture of membranes. Pak J Surg 2019; 35(1), 73-77